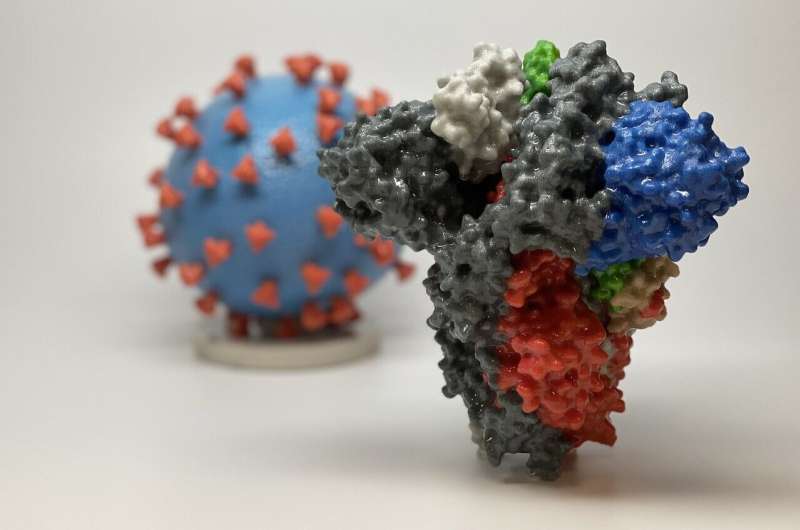
3D print of a spike protein of SARS-CoV-2, the virus that causes COVID-19—in front of a 3D print of a SARS-CoV-2 virus particle. The spike protein (foreground) enables the virus to enter and infect human cells. On the virus model, the virus surface (blue) is covered with spike proteins (red) that enable the virus to enter and infect human cells. Credit: NIH
It has been more than 11 months since we learned that a new and deadly virus was attacking the people of Wuhan, China.
Since then, more than 63 million people have been infected worldwide, and nearly 1.5 million have died.
Yet there are still a surprising number of unanswered questions about whether millions of COVID-19 survivors have found at least one silver lining: immunity.
President Trump famously declared that he was immune after his bout with the disease. Sen. Rand Paul (R-Ky.), who tested positive for the virus in March, last month said authorities should tell survivors, "to throw away their masks, go to restaurants, live again, because these people are now immune."
This is very much NOT how experts on immunity say you should behave after you've tested positive, but there is new evidence that important markers of immunity remain strong months after infection. That does not necessarily mean that survivors can't get sick again or spread the virus unwittingly while asymptomatic, hence the continuing advice to wear masks and keep your distance after recovery.
"We don't know enough about that scenario, "said John Wherry, an immunologist and director of the Penn Institute of Immunology. "We have to be very, very careful about changing behavior based on previous infection."
The question of how immunity to this virus works is of increasing importance for a nation that appears on the cusp of approving at least two COVID-19 vaccines on an emergency basis. At a meeting last month of the Advisory Committee on Immunization Practices (ACIP), which makes recommendations on vaccines to the U.S. Centers for Disease Control and Prevention, members wondered whether people who have had the disease recently could wait for their shots while others got the first, scarce doses. The group did not make a decision on that.
Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, has said he thinks that COVID-19 survivors should still get vaccinated.
Because these vaccines are brand new, we don't know how long the immunity they provide will last either. John Zurlo, an infectious diseases doctor at Jefferson Health, said it's not a huge problem if COVID-19 vaccines last only, say, a year. We're already accustomed to getting flu shots annually.
One reason scientists have feared that natural protection from COVID-19 might be short-lived is that immunity to milder coronaviruses that cause colds is fleeting. On the other hand, recent research found that the immune systems of survivors of SARS, a much more serious type of coronavirus, still had cells primed to fight the virus 17 years later.
Early in the coronavirus pandemic, there was evidence that infected people produced large numbers of antibodies, proteins that would recognize a new coronavirus invasion and prevent infection. However, the number of these antibodies fell after a few months.
Since then, more work has focused on B cells, which produce antibodies, and two types of T cells that either kill infected cells or help support the immune response. T cells go to work after the virus begins replicating. That means the virus can be active even while the immune system is reacting and could be contagious.
A recent study by the La Jolla Institute for Immunology that has not yet been vetted by a medical journal found reason to hope that survivors may have lasting immunity.
It looked at all these components of immunity up to eight months after infection and found that some of these "memory" cells responded to the coronavirus, or parts of it, in more than 90% of people, said Daniela Weiskopf, an immunologist who participated in the study. "This is good news," she said. The decline in response was slow, a sign that immunity could last a long time. But Weiskopf emphasized that "nobody knows" how things will look in a year or 18 months.
However, she said, the team was looking only at the ingredients for an immune reaction in a laboratory test. They don't know whether these memory cells actually keep people from getting sick, although there's good reason to believe they would.
There was wide variation in how many of the various cells or proteins individuals had. Researchers do not know how that might correlate with the degree of protection.
Weiskopf said the La Jolla study did not analyze immune system differences among specific demographic groups. There are questions about how well groups that have suffered most with the coronavirus—people over 65 and those with obesity and other chronic health problems—develop immunity. These groups tend to have weaker immune systems that may not respond as well either to vaccines or the virus itself. While older people tend to get less benefit from flu shots than the young, vaccine experts have been heartened to see that they respond well to the most recent shingles vaccine, Shingrix.
The study also did not look at whether the degree of later immune readiness correlated with how sick the virus initially made people.
Clearly, not everyone is protected, either by vaccines or getting sick. The first two vaccine candidates, made by Pfizer and Moderna, protect 94% to 95% of people. That means some still got sick.
Worldwide, there have been less than 30 cases of known re-infection among COVID-19 survivors, although more are suspected. Experts said the numbers would likely be much higher if most people had not developed immunity.
"I think that tells us that there's some level of immunity after you've recovered from the primary infection," Wherry said. "We don't know how durable that is."
It is too early to know whether natural immunity is better or different than immunity triggered by vaccines.
Zurlo said the latest surge in cases will be a test of natural immunity. He's waiting to see if there's a big increase in reported re-infections.
"In the end, the proof is in the clinical outcomes," he said. "I don't know that there's any way to rush that along, to be honest with you."
Thomas Fekete, an infectious diseases doctor and chair of medicine at the Lewis Katz School of Medicine at Temple University, is also keeping an eye on re-infections. The small number he said, is "slightly reassuring. The longer we don't have that happen, the better I'll feel."
He said he tells patients who have had COVID-19 that they probably have some protection, but that they should watch for reports of mutations in the virus that could affect immunity.
©2020 The Philadelphia Inquirer, LLC. Visit at inquirer.com. Distributed by Tribune Content Agency, LLC.