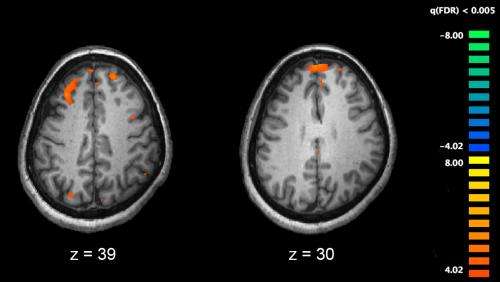
Functional magnetic resonance imaging (fMRI) and other brain imaging technologies allow for the study of differences in brain activity in people diagnosed with schizophrenia. The image shows two levels of the brain, with areas that were more active in healthy controls than in schizophrenia patients shown in orange, during an fMRI study of working memory. Credit: Kim J, Matthews NL, Park S./PLoS One.
Neurological soft signs (NSS) have been shown to be the important biomarkers for schizophrenia. These signs, including motor coordination, sensory integration and disinhibition, were conventionally thought to be minor neurological anomalies without any specific brain regions corresponding for the observed behavioral manifestations. Accumulating imaging findings have suggested these signs are actually associating with specific brain functional network. However, most of these studies have specifically focused on the association of motor coordination signs in patients with schizophrenia and general brain functional connectivity within the cerebral cortex.
More recently, evidence suggests that the cerebellum plays an important node in multiple function networks accounting for various cognitive and perceptual impairments observed in patients with schizophrenia. However, little is known about the underlying cerebellar-cerebral functional connectivity associating with sensory integration signs in patients with schizophrenia.
Dr. Raymond Chan and his team from the Institute of Psychology of the Chinese Academy of Sciences have shown that cerebellar hypoactivation was associated with sensory integration in patients with schizophrenia and their unaffected siblings.
Importantly, the cerebellar activation underlying sensory integration is heritable. Based on these findings, Dr. Chan and his team have recently conducted another study to further examine the specific relationship of NSS and cerebellar-cerebral resting-state functional connectivity (rsFC) in 51 patients with schizophrenia and 50 healthy controls.
Their findings showed that positive correlations between NSS and rsFC of the cerebellum with the inferior frontal gyrus and the precuneus, and negative correlations between NSS and rsFC of the cerebellum with the inferior temporal gyrus in patients with schizophrenia.
Moreover, they also found that cerebellar-prefrontal rsFC was also positively correlated with negative symptoms in schizophrenia patients. More importantly, similar findings were replicated in another sample of 34 patients with schizophrenia and 34 healthy controls.
"These findings demonstrate the important role of cerebellum and its connection to cerebral cortex contributing to both the NSS manifestations and negative symptoms in patients with schizophrenia. Such altered cerebellar-cerebral functional connectivity may share the same neural mechanism for NSS and negative symptoms in this clinical group," said Dr. Chan.
Besides, the cerebellar activation underlying sensory integration is heritable that suggested its role as a candidate endophenotype of schizophrenia.
This study has been published online in a paper entitled "Neurological soft signs are associated with altered cerebellar-cerebral functional connectivity in schizophrenia" in Schizophrenia Bulletin on Jan. 22, 2021.
More information: Xin-Lu Cai et al. Neurological Soft Signs Are Associated With Altered Cerebellar-Cerebral Functional Connectivity in Schizophrenia, Schizophrenia Bulletin (2020). DOI: 10.1093/schbul/sbaa200
Provided by Chinese Academy of Sciences