February 25, 2021 feature
Wireless, implantable catheter-type oximeter designed for cardiac oxygen saturation
The real-time monitoring of intravascular oxygen levels is important to accurately track the cardiopulmonary health of patients after cardiothoracic surgery. Existing methods use intravascular placement of glass fiber-optic catheters that pose risks of blood vessel damage, thrombosis and infection. Physical tethers to power supply systems can limit freedom of movement in the intensive care unit. In a new report now on Science Advances, Wei Lu and a team of international researchers in multidisciplinary research across the U.S., China, the Republic of Korea and Italy introduced a wireless, miniaturized and implantable optoelectronic catheter system. The device included optical components on the probe, encapsulated by soft biocompatible materials. The flexible, biocompatible construction of the probe represented key defining features to form a high-performance, patient-friendly oximeter that could monitor localized tissue oxygen, heart rate and respiratory activity in real time. The platform offered measurement accuracy and precision similarity to existing chemical standards.
The cardiovascular system
The cardiovascular system delivers oxygen and nutrients to tissues and cells in the body and maintains an adequate balance between oxygen delivery and consumption for cellular physiological function. The accurate and real-time monitoring process of specific intracardial and major vascular saturations after open-heart surgery is critical to treat patients suffering from cyanotic congenital heart defects. Wearable oximeters and clinical pulse oximeters can capture global oxygenation of the body. In the intensive care unit (ICU) setting, the fiber-optic oximetric catheter can be used to monitor blood oxygen saturation levels continuously. With existing fiber-optic catheter oximetry, clinicians incorporate hard glass fiber waveguides to connect to a light source and sensing module to deliver light form an external source to the blood at the tip of the catheter in order to transmit some fractions of the backscattered light back to an external unit for detection. The apparatus can be connected to an additional interface containing a display monitor and controlling software. The platform introduced in this work contained a thin, flexible catheter-type optoelectronic probe connecting to a small, wearable electronic module for wireless and continuous real-time measurements of intravascular oxygen with clinical-grade accuracy.
Design features
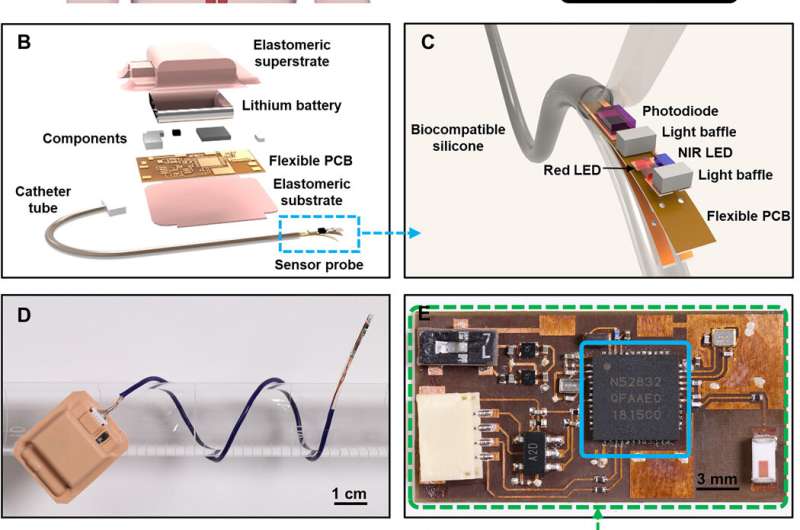
The probe tip of the device contained high-performance, miniaturized light-emitting diodes (LEDs) and photodiode (PD) fully encapsulated with a medical-grade, soft, transparent silicone elastomer. The electronic module supported rechargeable powering, circuit control and wireless data communication via Bluetooth protocols. A graphical user interface (GUI) deployed on a smartphone or tablet computer of ICU monitoring display allowed real-time visualization storage and analysis of measurement data. The results represented important advances in wireless optoelectronic technologies in cardiology. The platform was fully encapsulated with a medical-grade silicone layer and contained three main components:
- A low modulus flexible catheter with an optoelectronic sensor that contained two light-emitting diodes with emission wavelengths of 645 and 950 nm and one silicone photodiode.
- A bendable, miniaturized Bluetooth electronic module for gentle mounting on the skin
- A custom GUI deployed on a handheld device to support real-time visualization storage and data analysis and provide a control interface for the illumination parameters for LEDs.
The team then wirelessly transferred data to a personal computer using Bluetooth protocols.
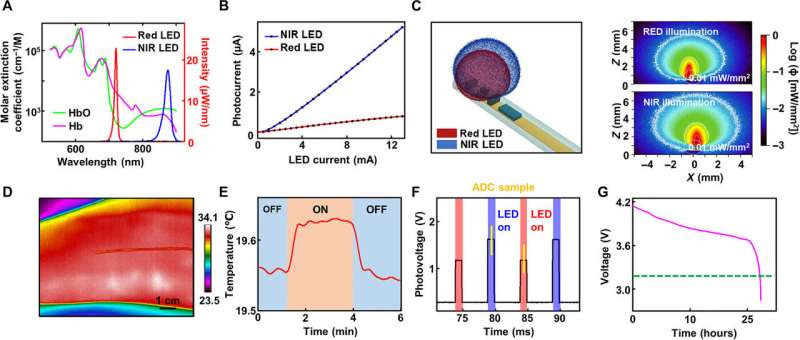
Optical, thermal and electrical characterization
The scientists provided effective estimates of blood oxygen saturation using well-known optical approaches to define the fraction of oxyhemoglobin (HbO2) relative to total hemoglobin (HbO2 + deoxyhemoglobin—Hb) by comparing the absorption spectra of oxyhemoglobin and deoxyhemoglobin in the visible and near-infrared spectral range. Using the large differences at 645 nm and 950 nm, the scientists established the basis of optical measurements of blood oxygenation. Lu et al. measured the physics of light transport in biological tissues using the Monte Carlo method. The results provided quantitative insights into the illumination distribution around the LEDs and into aspects of light detection by the photodiode based on the optical properties of human cardiac muscle tissue found in literature. While the device functioned when pressed against the skin of the fingertips, Lu et al. obtained thermal images with an IR camera, which did not show apparent increase in temperature in the region. The scientists performed measurements every five minutes for a duration of five seconds.
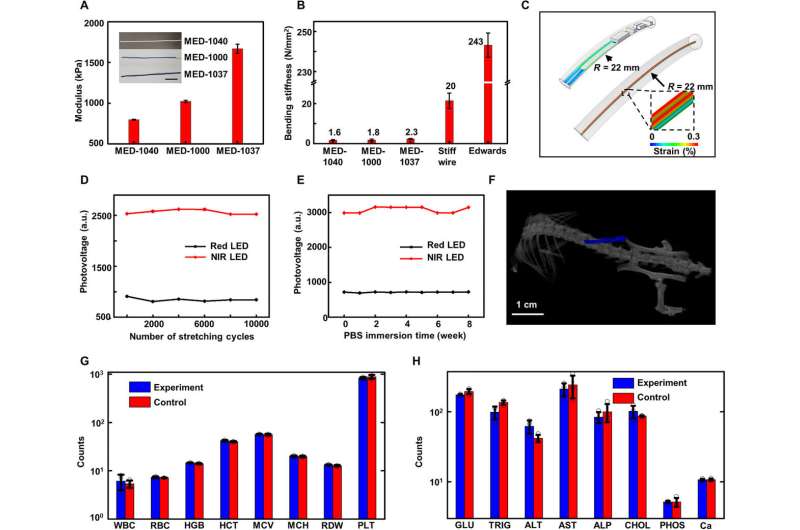
Mechanical characterization and encapsulation performance
The mechanical properties of the device minimized the mechanical forces on adjacent biological tissues for improved biocompatibility. Human skin typically maintains a Young's modulus or stiffness between 400 and 800 kPa and human cardiac tissue muscles have a Young's modulus approximating 100 kPa. The Bluetooth module contained a biocompatible silicone for encapsulation with a Young's modulus in the range of human skin. The team used three catheter oximeter probes with biocompatible silicone with diverse Young's modulus values. The resulting bending stiffness of the construct was 50 times greater than that of the probe. The probe could easily and conformally deform with the heart muscle with negligible mechanical load and without associated damage to the heart, although its modulus was greater. Lu et al. implanted the device subdermally on the back near the spine of a mouse model and conducted computed tomography two weeks later. The team then obtained complete blood count and blood chemistry for mice with implants for 30 days to indicate no evidence of organ damage or injury and without detrimental effects on electrolyte or enzyme balance.
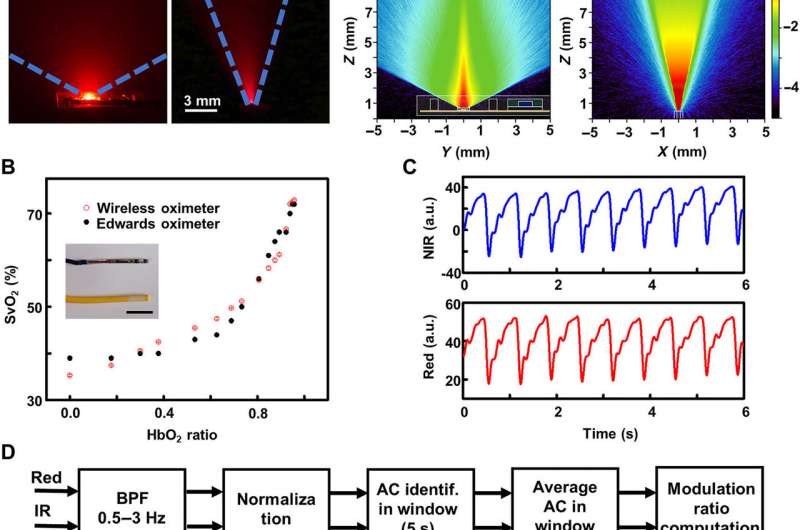
Bench tests and in vivo studies
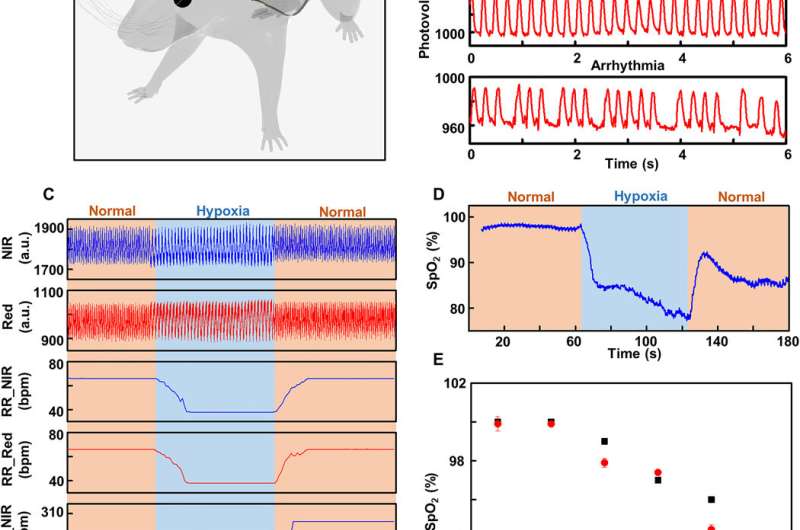
Major cardiac surgeries rely on the monitoring of venous oxygen saturation (SvO2) and central venous oxygen saturation (ScvO2) measured using fiber-optic oximeters to guide care. Such devices can be implanted transvenously to support the optical transmission from external sources across to sense with detectors in a patient tethered to a bedside apparatus. The team conducted in-lab tests using horse blood at various oxygen levels and compared those with commercial systems. The results showed measurement capabilities of SvO2 and ScvO2 across relevant ranges. The method can be implemented in pediatric cardiac surgery and recovery to monitor oxygen saturation levels within vessels during early and critical post-operative period in real time. Lu et al. conducted experiments on rat models and the device captured changes in HR, respiration rate (RR), ischemia and arrhythmia. The team also measured the heart rate and respiration rate during the experiments. The high degree of correlation demonstrated that the device offered sufficient sensitivity and precision in real-time oxygenation monitoring.
Outlook
In this way, Wei Lu and colleagues used a flexible, thin, catheter-type oximeter to accurately monitor venous and cardiac oxygenation levels in real time. The results demonstrated a wireless optoelectronic platform at the millimeter-scale to detect cardiac oxygenation saturation in rats during open-heart surgery. They explored the potential of the device to monitor oxygen levels in main vessels and expect to conduct further studies on the efficiency and reliability of oxygen saturation detection in large animal models to mimic open heart surgery of patients.
More information: Liu W. et al. Wireless, implantable catheter-type oximeter designed for cardiac oxygen saturation, Science Advances, DOI: 10.1126/sciadv.abe0579
McGee D. C. et al. Preventing complications of central venous catheterization. New England Journal of Medicine. 10.1056/NEJMra011883
Lee K. et al. Mechano-acoustic sensing of physiological processes and body motions via a soft wireless device placed at the suprasternal notch, Nature Biomedical Engineering, doi.org/10.1038/s41551-019-0480-6
© 2021 Science X Network



















