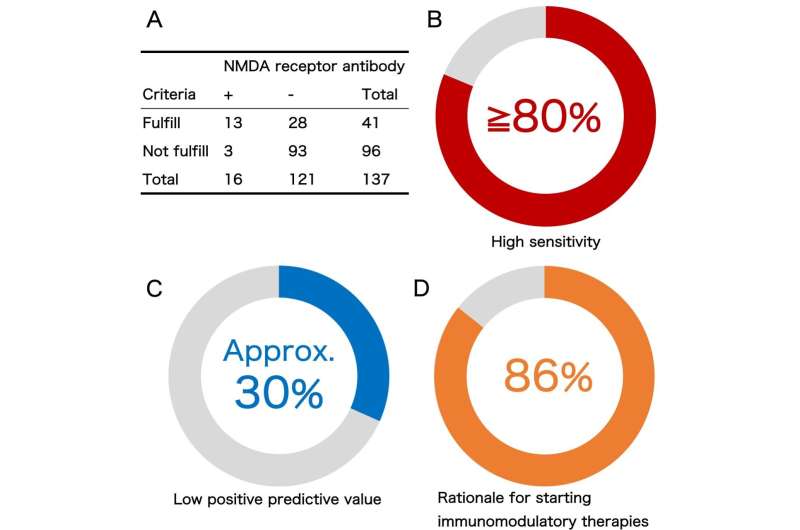
The results of evaluation of the clinical diagnostic criteria for anti-NMDA receptor encephalitis in Japanese children are summarized (A-D). Total of 137 patients including 16 patients with positive anti-NMDA receptor antibody were included in the study (A). Over 80% of antibody-positive patients fulfill the criteria, suggesting the clinical diagnostic criteria has high sensitivity (B), however, only about 30% of the children who fulfill the criteria actually tested positive in the antibody analysis in our cohort (C). Most of the children without the antibody, but fulfilled the criteria (false positive cases) were diagnosed with a neuroimmunological disease (D). Collectively, physicians should start immunomodulatory therapy when their patients fulfill the diagnostic criteria. Credit: TMIMS
Anti-NMDA receptor (NMDAR) encephalitis was first reported to develop in female young adults with ovarian teratoma. However, another study with a larger cohort reported that more than one-third of all patients with anti-NMDAR encephalitis were aged under 18 years, suggesting that this encephalitis might be more common in children than originally expected.
A clinical diagnostic approach to autoimmune encephalitis was proposed in 2016, and included diagnostic criteria for probable and definite anti-NMDAR encephalitis. For a diagnosis of probable anti-NMDAR encephalitis, the criteria require rapid onset (<3 months) of at least 4 of the 6 major symptom groups: (1) abnormal behavior or cognitive dysfunction; (2) speech dysfunction; (3) seizures; (4) movement disorders, dyskinesias, or rigidity/abnormal postures; (5) decreased level of consciousness; and (6) autonomic dysfunction or central hypoventilation. These criteria were established to promote early immunomodulatory therapy administration in patients with anti-NMDAR encephalitis, and thus require high sensitivity. The criteria have indeed been reported as highly sensitive and specific in both adult and pediatric patients; however, symptoms depend on age.
Adult patients tend to present with behavioral problems and often develop memory deficits and central hypoventilation. In contrast, central hypoventilation was observed in just 23% of patients younger than 18 years. Patients under 12 are more likely to present with seizures or movement disorders. Children may also show atypical symptoms, such as cerebellar ataxia or hemiparesis. Neurologic assessment is difficult in some pediatric patients. We therefore evaluated the validity of the criteria for anti-NMDAR encephalitis in a Japanese pediatric cohort.
We retrospectively reviewed clinical information of patients with neurologic symptoms whose CSF was analyzed for NMDAR antibodies (NMDAR-Abs) in our laboratory from January 1, 2015, to March 31, 2019.
Overall, 137 cases were included. Of the 41 cases diagnosed as probable anti-NMDAR encephalitis (criteria-positive) according to the 2016 criteria, 13 were positive and 28 were negative for anti-NMDAR-Abs. Of the 96 criteria-negative cases, 3 were positive and 93 were negative for anti-NMDAR-Abs. The sensitivity of the criteria was 81.2%, specificity was 76.9%, positive predictive value (PPV) was 31.7%, and negative predictive value was 96.9%. Compared with the true-positive group, the false-positive group contained more male than female patients (male:female, 4:9 in the true-positive vs 19:9 in the false-positive group, p = 0.0425). The majority of the cases with false-positive diagnoses were associated with neurologic autoimmunity.
The clinical diagnostic criteria are reliable for deciding to start immunomodulatory therapy in the criteria-positive cases. Low PPV may be caused by a lower prevalence of NMDAR encephalitis or lower level of suspicion for encephalitis in the pediatric population. Physicians should therefore continue differential diagnosis, focusing especially on other forms of encephalitis.
More information: Hiroya Nishida et al, Evaluation of the Diagnostic Criteria for Anti-NMDA Receptor Encephalitis in Japanese Children, Neurology (2021). DOI: 10.1212/WNL.0000000000011789
Journal information: Neurology
Provided by Tokyo Metropolitan Institute of Medical Science