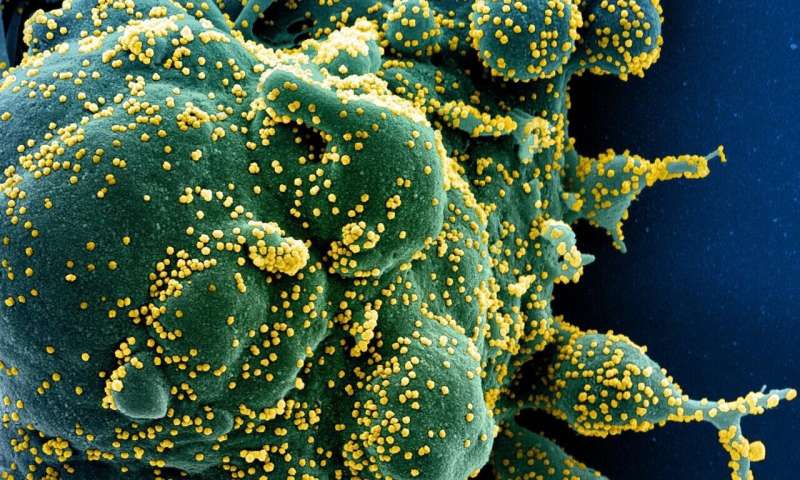
Colorized scanning electron micrograph of an apoptotic cell (green) heavily infected with SARS-COV-2 virus particles (yellow), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIH/NIAID
A new study published in The Lancet Infectious Diseases journal has found that the risk of delayed acute complications after non-hospitalized SARS-CoV-2 infection is low, but persistent symptoms in this group could lead to increased visits to general practitioners or outpatient clinics in the six months following infection. The study assessed only those complications that led to contact with hospitals.
Researchers assessed the risk of initiating medication and receiving a hospital diagnosis for a new condition by comparing individuals who tested positive via a PCR test for SARS-CoV-2 with individuals who had a negative test during the first wave of the pandemic in Denmark. Results found SARS-CoV-2 positive individuals were at a slightly increased risk of initiating medications to help improve breathing and alleviate migraines, and had a slightly increased risk of receiving a first diagnosis for breathing problems and blood clots in the veins.
Senior author, Professor Anton Pottegård from the University of Southern Denmark says: "Until now, most research investigating long-term complications from COVID-19 has been focused on hospitalized patients. But the reality is that the majority of people with COVID-19 are not admitted to the hospital. Our study finds a very low risk of severe delayed effects from COVID-19 in people who didn't require hospitalization for the infection. However, our research provided evidence for some long-term effects that did not require hospitalization or the use of new medicines, which we found reflected in higher use of primary health-care services after infection. This highlights the need to ensure clinicians have the resources and support to manage any potential long-term conditions."
The researchers used data from the Danish health registries on all individuals who were tested for SARS-CoV-2 between Feb 27, 2020, and May 31, 2020. The study followed up 8,983 non-hospitalized SARS-CoV-2 positive people and 80,894 SARS-CoV-2-negative people during the period from two weeks to six months after the test. By comparing data from the two groups, researchers assessed the relative risk of starting new medications and of receiving a diagnosis of a new health condition during this time.
The analysis took into account variables that could be associated with having a positive versus negative test and with the risk of a more severe course of COVID-19, such as obesity, cancer, and kidney disease.
The cohorts had a median age of 43 years and 64% were female. Among SARS-CoV-2 positive individuals, 31% had initiated new medication treatments during the follow up period. A more detailed analysis found that compared with those with a negative SARS-CoV-2 test those with a positive test were at an increased risk of initiating medications to widen the airways (1.8% compared with 1.5%), and medications to treat migraines (0.4% compared with 0.3%). As such, observed differences were generally small.
The risks of receiving a hospital diagnosis for a new health condition during follow up were similar in the two groups (around 26%). Compared with individuals who tested negative, those with a positive SARS-CoV-2 test were at an increased risk of receiving a first diagnosis of breathing difficulties (1.2% compared with 0.7%) and blood clots in the veins (0.2 % compared with 0.1%). No increased risk of serious complications identified by previous research conducted among individuals hospitalized for COVID-19, such as stroke, encephalitis, and psychosis, was identified among individuals who did not require hospitalization.
The research also analyzed the use of health services in the follow-up period and found that those with a positive SARS-CoV-2 test visited their general practitioners around 20% (1.2 times) more often than those that tested negative, and visited outpatient clinics 10% (1.1 times) more often. However, there was no difference in the visits to emergency department or being hospitalized.
The follow-up of the study was limited to six months after the positive test, which means the data may not have captured the longer-term complications and symptoms of COVID-19 that could occur after this time. In addition, due to the limited resources during the pandemic, some individuals with complications may have been referred to hospitals but not actually attended clinics before the end of the follow-up. This may have affected the numbers of hospital diagnoses recorded.
Commenting on the limitations of the study, co-author Stine Hasling Mogensen, Ph.D., from the Danish Medicines Agency adds: "Our analysis only captures specific symptoms leading to contact with hospitals, so it is likely that the study underestimates symptoms which do not require this level of care, like fatigue and breathing difficulties which are not severe enough for hospitalization or require initiation of new medical treatment. Previous research has found a high level of these symptoms reported by patients, so the differences between patient reports and healthcare encounters could be important to investigate in regards to potential unmet healthcare needs and the need for new medications for treatment."
The researchers call for large population-based studies of patient-reported symptoms and healthcare visits to fully evaluate the duration and range of any persisting symptoms after SARS-CoV-2 infection.
More information: Lars Christian Lund et al. Post-acute effects of SARS-CoV-2 infection in individuals not requiring hospital admission: a Danish population-based cohort study, The Lancet Infectious Diseases (2021). DOI: 10.1016/S1473-3099(21)00211-5
Journal information: Lancet Infectious Diseases
Provided by Lancet