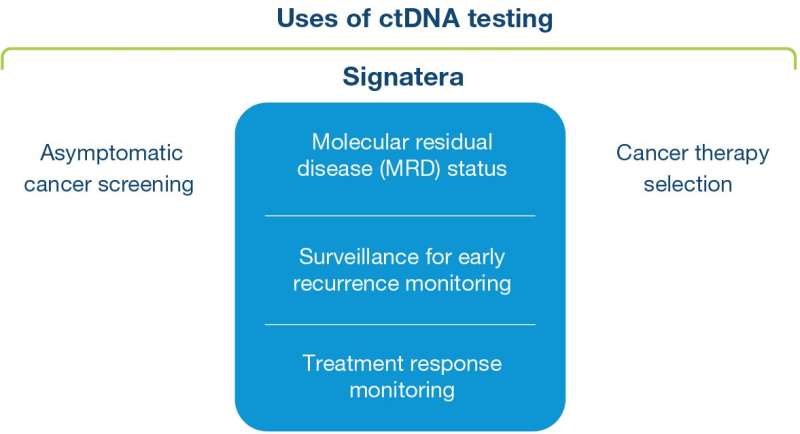
Utilizing the Signatera test, early detection of MRD has become a powerful tool for improving cancer management outcomes.
Four years ago, researchers in the CRUK TRACERx team at the Crick and UCL, alongside an industry-collaborator Natera, developed a personalized test that uses circulating fragments of tumor DNA (ctDNA) in the blood of patients with lung cancer to predict if their cancer would come back after surgery - even before it would be visible on a scan. And last week, a personalized and tumor-informed blood test called Signatera proved effective at defining which patients will benefit from immune therapy after surgery in a landmark clinical trial. Charles Swanton, head of the Cancer Evolution and Genome Instability Laboratory at the Crick and UCL, and Chief Clinician at Cancer Research UK, explains how this technology evolved from an idea into a potentially life-saving clinical test.
Caring for patients with cancer can be incredibly rewarding. We've seen amazing progress in recent years, with new tests and therapies that enable us to successfully treat and manage the disease for more people. But significant challenges remain.
Tumors evolve over time, adapting to their surroundings, becoming resistant to treatments and spreading to other parts of the body. We and others have reasoned that the earlier disease relapse can be detected, the smaller the burden of disease and the greater the chance that treatments will be effective.
This is why we started TRACERx, a Cancer Research UK funded study to track lung cancer evolution in real time, looking at how genetic changes and diversity within tumors affects the course of disease. We've followed hundreds of patients, from diagnosis through to either disease relapse or cure after surgery, tracking and analyzing how their cancer has developed.
In one of our studies from 2017, we showed that we could use the patchwork of genetic faults, defined through gene-sequencing of a patient's lung tumor tissue, as a cancer fingerprint. We showed that this fingerprint could help identify remnants of that patient's cancer following surgery through a simple blood test. In some cases, we could detect relapsing cancer many months before doctors caring for that patient found that same cancer on routine follow-up scans.
The ctDNA test is based upon patient-specific genetic mutations, present in every part of their tumor. Amplifying these unique markers makes it easier to detect a minimal amount of residual disease—the needle in the haystack that's almost impossible to spot.
And just last week we had the news that all researchers hope for. The validation of this ground-breaking technology has helped improve outcomes for patients.
In a landmark clinical trial led by Dr. Thomas Powles at Barts Cancer Institute, researchers performed Signatera ctDNA tests in over 500 patients who had received surgery to remove tumors in the bladder or urinary system. Patients were randomized to receive monitoring or additional treatment with an immunotherapy drug atezolizumab. Patients positive for ctDNA had improved overall survival if they were given atezolizumab, but the same benefit wasn't seen for patients without ctDNA in their blood.
This means the test can be used to accurately identify patients most likely to benefit from additional treatment, and importantly survive for longer. Not only will this increase the number of people surviving their cancer, but spare others unnecessary treatments and related side effects.
The possible benefits don't end here. These types of tests have the potential to completely transform the way we treat patients following surgery. Traditionally, we use pathological information about tumor stage to guide whether we offer additional treatments like chemotherapy after surgery to eradicate residual tumor cells that may spread one day, and minimize the risk of recurrence. But now, there is the real potential that treatment may be refined and guided by molecular tests such as these, offering therapy only to those patients who will really benefit from it.
We could see an end to the anxious wait patients face between follow-up scans, wondering whether their treatment has worked or if their cancer has come back. With further validation in different cancer types, we could also use this test to monitor response to treatments in the absence of disease on a scan, changing tack at the earliest sign of drug resistance.
None of this would be possible without the foundation of biological research—the fundamental understanding of tumor genetics and evolution that has led to more refined and personalized tests and treatments. I have no doubt that in the not too distant future, we will see cancer treatment plans informed through personalized genetic testing and regular monitoring of tumor DNA in the blood.
Provided by The Francis Crick Institute