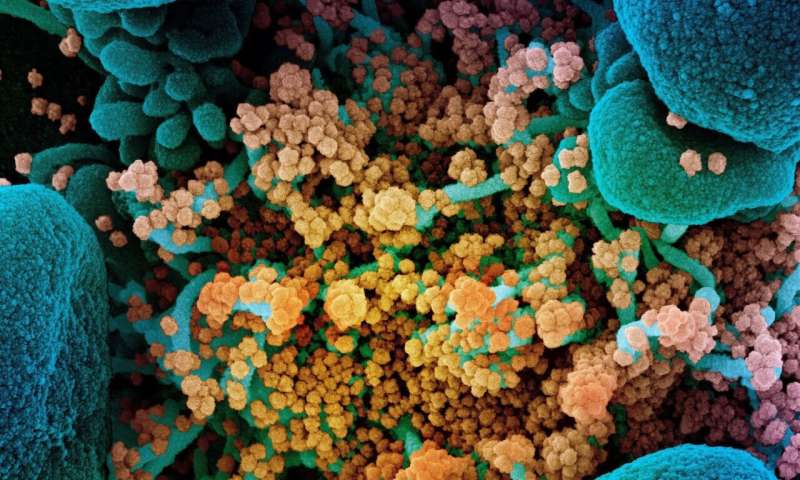
Colorized scanning electron micrograph of a dying cell (blue) heavily infected with SARS-CoV-2 (yellow), the virus that causes COVID-19. Credit: NIAID Integrated Research Facility, Fort Detrick, Maryland.
When a person is infected with SARS-CoV-2, the virus that causes COVID-19, it invades their cells and uses them to replicate—which puts the cells under stress. Current approaches to dealing with infection target the virus itself with antiviral drugs. But Cambridge scientists have switched focus to target the body's cellular response to the virus instead.
In a new study, published today in the journal PLOS Pathogens, they found that all three branches of a three-pronged signalling pathway called the 'unfolded protein response' (UPR) are activated in lab-grown cells infected with SARS-CoV-2. Inhibiting the UPR to restore normal cell function using drugs was also found to significantly reduce virus replication.
"The virus that causes COVID-19 activates a response in our cells—called the UPR—that enables it to replicate," said Dr. Nerea Irigoyen in the University of Cambridge's Department of Pathology, senior author of the report.
She added: "Using drugs we were able to reverse the activation of this specific cellular pathway, and remarkably this reduced virus production inside the cells almost completely, which means the infection could not spread to other cells. This has exciting potential as an anti-viral strategy against SARS-CoV-2."
Treatment with a drug that targets one prong of the UPR pathway had some effect in reducing virus replication. But treatment with two drugs together—called Ceapin-A7 and KIRA8—to simultaneously target two prongs of the pathway reduced virus production in the cells by 99.5%. This is the first study to show that the combination of two drugs has a much greater effect on virus replication in cells than a single drug.
The approach would not stop a person getting infected with the coronavirus, but the scientists say symptoms would be much milder, and recovery time would be quicker.
Anti-viral drugs currently in use to treat COVID-19, such as remdesivir, target replication of the virus itself. But if the virus develops resistance to these drugs they will no longer work. In contrast, the new treatment targets the response of the infected cells; this will not change even if new variants emerge, because the virus needs this cellular response in order to replicate.
The next step is to test the treatment in mouse models. The scientists also want to see whether it works against other viruses, and illnesses such as pulmonary fibrosis and neurological disorders that also activate the UPR response in cells.
"We hope this discovery will enable the development a broad-spectrum anti-viral drug, effective in treating infections with other viruses as well as SARS-CoV-2. We've already found it has an effect on Zika virus too. It has the potential to have a huge impact," said Irigoyen.
SARS-CoV-2 is the novel coronavirus responsible for the COVID-19 pandemic. Since the end of 2019 there have been over 150 million cases of the disease worldwide, and over 3 million people have died.
More information: PLOS Pathogens (2021). DOI: 10.1371/journal.ppat.1009644
Journal information: PLoS Pathogens
Provided by University of Cambridge