Molecular imaging improves staging and treatment of pancreatic ductal adenocarcinomas
For patients with pancreatic ductal adenocarcinomas (PDAC), molecular imaging can improve staging and clinical management of the disease, according to research published in the June issue of The Journal of Nuclear Medicine. In a retrospective study of PDAC patients, the addition of PET/CT imaging with 68Ga-FAPI led to restaging of disease in more than half of the patients, most notably in those with local recurrence.
PDAC is a highly lethal cancer, with a five-year survival rate of less than 10 percent. Optimal imaging of PDAC is crucial for accurate initial TNM (tumor, node, metastases) staging and selection of the primary treatment. Follow-up imaging is also important to accurately detect local recurrence or metastatic spread as early and as completely as possible.
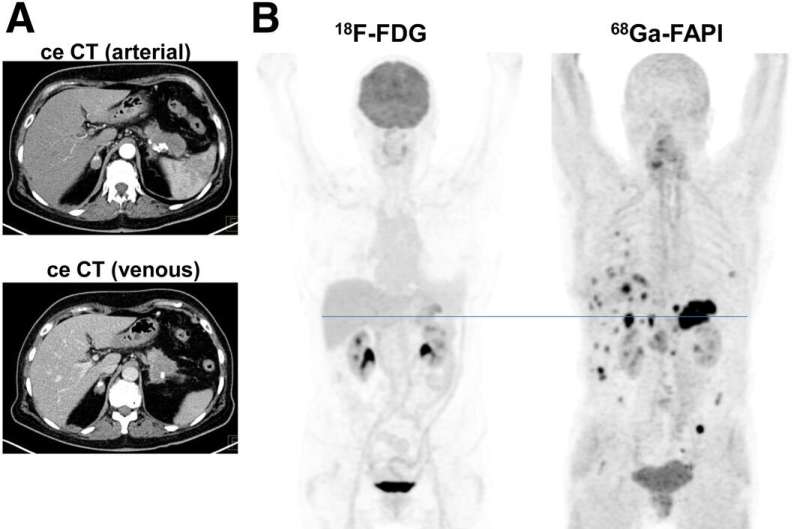
"Currently, contrast-enhanced CT is the gold standard when it comes to TNM staging, and PET imaging isn't typically part of the clinical routine" stated Manuel Röhrich, MD, nuclear medicine physician at Heidelberg University Hospital in Heidelberg, Germany. "However, we know that PDAC is composed of certain fibroblasts that express fibroblast activation protein, which can be imaged with the novel PET radiotracer 68Ga-FAPI. Given this characteristic, we sought to explore the utility of 68Ga-FAPI PET/CT to image FDAC patients."
The study included 19 FDAC patients who received contrast-enhanced CT imaging followed by 68Ga-FAPI PET/CT. Results from the 68Ga-FAPI PET/CT scans were then compared with TNM staging based on contrast-enhanced CT. Changes in oncological management were recorded.
68Ga-FAPI PET/CT-based TNM staging differed from contrast-enhanced CT imaging in 10 out of 19 patients, which resulted in changes in TNM staging. Of the 12 patients with recurrent disease, eight were upstaged, one was downstaged and three remained the same. In the seven patients newly diagnosed with PDAC, one was upstaged, while the staging remained the same for six of the patients.
"This analysis suggests that 68Ga-FAPI PET/CT is a promising new imaging modality in staging of PDAC that may help to detect new or clarify inconclusive results obtained by standard CT imaging," said Röhrich. He added, "Improvement in survival can only be achieved by effective treatment approaches customized to the individual patient's disease status. Thus, hybrid imaging using FAPI tracer may open up new applications in staging and restaging of PDAC."
More information: Manuel Röhrich et al, Impact of 68Ga-FAPI PET/CT Imaging on the Therapeutic Management of Primary and Recurrent Pancreatic Ductal Adenocarcinomas, Journal of Nuclear Medicine (2020). DOI: 10.2967/jnumed.120.253062



















