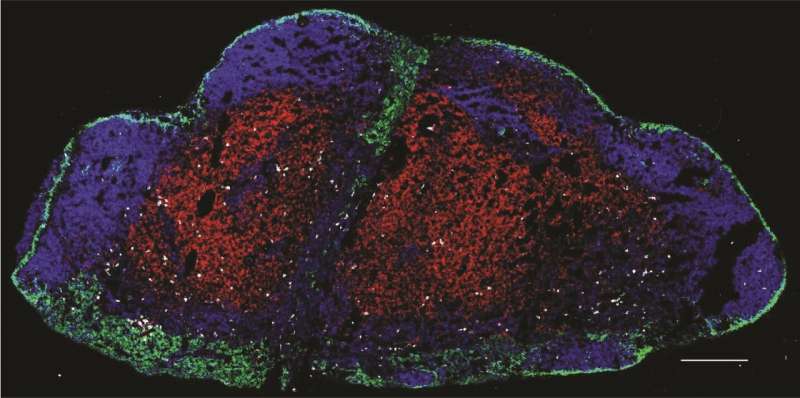
Microscopic image of tumor-specific resident memory T cells (white) stationed throughout a mouse tumor-draining lymph node. Researchers have found this novel population of long-lived T cells that stay in lymph nodes where they provide protection against melanoma. Credit: Dartmouth's Norris Cotton Cancer Center.
In the progressing field of immunotherapy, surprisingly little is known about immunity to metastatic tumors in locations such as lymph nodes, a frequent place where cancers first spread. Not only do lymph nodes act as a gateway for cancer cells to travel throughout the body, but they are also home to infection-fighting white blood cells called T cells. In some cases, T cells in lymph nodes activate to kill invading cancer cells. In other cases, that process clearly fails.
To address the need to understand why, researchers in the laboratory of Mary Jo Turk, Ph.D., Co-Director of the Immunology and Cancer Immunotherapy Research Program at Dartmouth's and Dartmouth-Hitchcock's Norris Cotton Cancer Center (NCCC) have spent the past year studying immunity to metastatic cancer within lymph nodes.
While T cells can freely travel from lymph nodes into the bloodstream and back to the lymph nodes, researchers in Turk's lab have discovered a novel population of tumor-fighting T cells that do not circulate, but rather stay in lymph nodes where they provide protection against melanoma. "These T cells, for whatever reason, have changed their program and stay in the lymph nodes where they persist and kill tumor cells for many months while never entering circulation," says Turk.
These long-lived T cells, called "lymph node resident memory T cells," were shown to counteract melanoma spreading in mice. Turk's team found that when melanoma cells were put back into mice that had been cured of cancer with immunotherapy a month earlier, the lymph nodes were still resistant to the cancer—the melanoma would not grow.
"We also identified T cells with similar characteristics in melanoma-invaded patient lymph nodes, showing that similar populations exist in humans," reveals Turk.
Computational analysis of melanoma specimen data from The Cancer Genome Atlas revealed that the presence of T cells with this gene signature predicted better outcomes and improved survival for human melanoma patients with lymph node metastases. "These studies reveal a new population of T cells that is vital for counteracting the earliest stages of cancer metastasis," says Turk.
Although the concept of T cells taking up residence in lymph nodes is not entirely new, it has never been shown in cancer. The team's findings, "Resident memory T cells in regional lymph nodes mediate immunity to metastatic melanoma," are newly published in Immunity.
The team, including clinicians at Dartmouth-Hitchcock Medical Center, as well as researchers at Baylor College of Medicine led by computational biologist, Chao Cheng, Ph.D., employed innovative sequencing techniques to identify the unique transcriptional profile that makes these resident T cells specific to lymph nodes and to cancer. "We found that these cells have a unique gene expression profile that differentiates them from cells in circulation, and from memory T cells that reside in and protect other tissues such as the skin," says Cheng.
Other collaborators on this work include the University of Michigan and University of Texas, San Antonio.
In the coming year, the Turk research team hopes to better understand how these memory T cells are most effectively generated and activated within lymph nodes. The ultimate goal is to understand how memory T cells can be positioned throughout tissues to efficiently block cancer from spreading.
More information: Resident memory T cells in regional lymph nodes mediate immunity to metastatic melanoma, Immunity, DOI: 10.1016/j.immuni.2021.08.019
Journal information: Immunity
Provided by Dartmouth-Hitchcock Medical Center