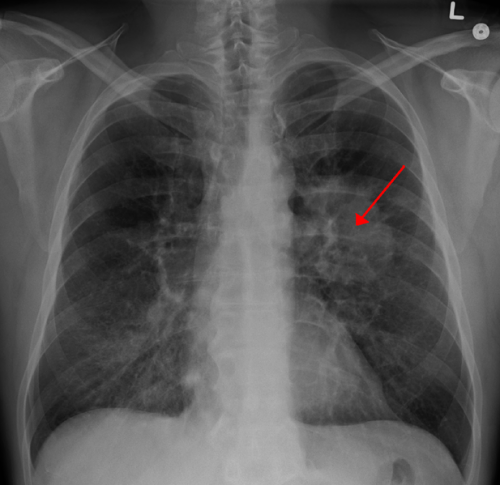
Lung CA seen on CXR. Credit: CC BY-SA 4.0 James Heilman, MD/Wikipedia
The Phase III IMpower010 trial evaluating atezolizumab vs. best supportive care after surgical resection and adjuvant chemotherapy met its primary endpoint showing significant disease-free survival improvement for patients with stage II-IIIA (UICC v7) non-small cell lung cancer. Study results were presented today at the IASLC 2021 World Conference on Lung Cancer.
At the interim disease-free survival analysis, the trial's primary endpoint, showed a significant disease-free survival benefit with atezolizumab compared with best supportive care after complete resection and adjuvant chemotherapy in patients with PD-L1 TC ≥1% stage II-IIIA NSCLC and in all randomized patients with stage II-IIIA NSCLC; the significance boundary for disease-free survival was not crossed in the intent-to-treat (ITT) population (stage IB-IIIA NSCLC).
Atezolizumab was well tolerated, and no new safety signals were identified. In their current presentation, the investigators examined the impact of therapies prior to adjuvant atezolizumab, including the extent of pulmonary resection, the type of mediastinal nodal assessment and adjuvant chemotherapy regimens, on disease-free survival. These pre-randomization variables as well as the time from surgery to adjuvant treatment are topics of interest, according to Nasser Altorki, M.D., of New York-Presbyterian Hospital, Weill Cornell Medicine in New York City.
Altorki and co-investigators across 22 countries and regions enrolled 1280 patients with completely resected stage IB (tumors ≥4 cm)-IIIA NSCLC (AJCC/UICC v7) and an ECOG performance status of 0-1. Patients received up to four 21-day cycles of cisplatin-based chemotherapy, and 1005 patients were subsequently randomized 1:1 to atezolizumab 1200 mg every three weeks (16 cycles or until disease recurrence or unacceptable toxicity) or best supportive care. The primary endpoint of investigator-assessed disease-free survival was tested hierarchically in the PD-L1 TC ≥1% (SP263) stage II-IIIA population, all-randomized stage II-IIIA population, and ITT population (stage IB-IIIA).
Surgery type, disease stage, mediastinal nodal assessment, and cisplatin-based chemotherapy regimens were well balanced between the atezolizumab and best supportive care arms. In the ITT population, the most common surgery was lobectomy (78.1%); 15.9% had pneumonectomy and 5.0% had bilobectomy. Mediastinal lymph node dissection or sampling was performed in 80.7% and 18.0% of patients, respectively. The majority of patients (76%-95%) across different chemotherapy treatments in both arms received the planned 4 cycles of chemotherapy.
In the ITT population, median time from surgery to first atezolizumab treatment or best supportive care was 5.2 months (range, 2.4-7.7) and 5.1 months (range, 2.3-8.0), respectively. In this exploratory analysis, the forest plots showed that disease-free survival in the PD-L1 TC ≥1% stage II-IIIA and all-randomized stage II-IIIA populations favored the atezolizumab vs. best supportive care arm across most disease stages, surgery types, and chemotherapy regimens.
"Patients who participated in the IMpower010 trial, including patients with nodal involvement, saw benefit across disease stages (stage II-IIIA sub-populations)," Altorki reported.
Provided by International Association for the Study of Lung Cancer