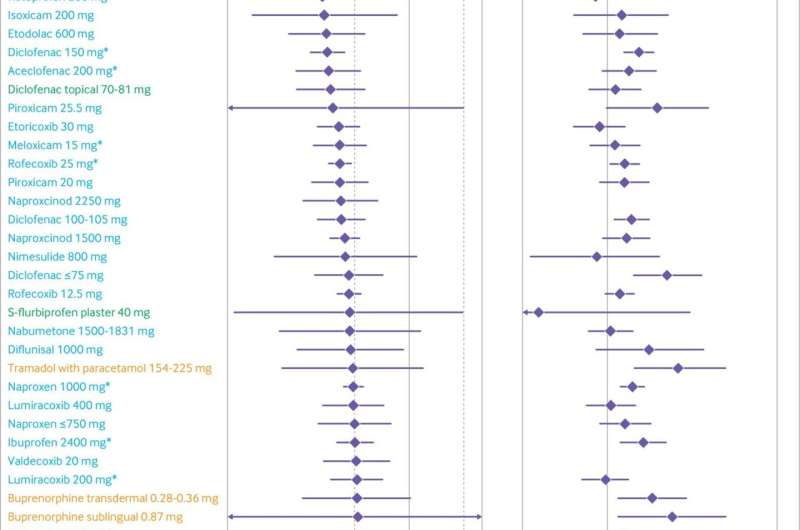
Treatment effect on osteoarthritis pain and dropouts due to adverse events compared with oral placebo, ordered according to treatment effect size on osteoarthritis pain. Blue: oral non-steroidal anti-inflammatory drugs; green: topical non-steroidal anti-inflammatory drugs; orange: opioids. Area between dashed lines shows treatment effect estimates below the minimum clinically important difference. See web-appendix 17 for caterpillar plot ordered according to odds ratio of dropouts due to adverse events. Credit: DOI: 10.1136/bmj.n2321
Topical medication for pain relief is safer and more effective than opioids in treating knee osteoarthritis pain, according to a meta-analysis by Unity Health Toronto researchers.
The paper, published in BMJ, compared the benefits and harms of different doses of commonly prescribed treatments for hip and knee osteoarthritis, including oral non-steroidal anti-inflammatory drugs (NSAIDs), topical NSAIDs, opioids, and acetaminophen (Tylenol). The meta-analysis looked at 192 large, randomized clinical trials comprising of over 102,000 participants.
Researchers found, regardless of preparation or dose, opioids did not significantly relieve pain for osteoarthritis patients. They also found that topical Diclofenac—known to consumers as Voltaren—is effective in treating knee osteoarthritis.
The topical treatment, which can be purchased over-the-counter, is generally safer than oral NSAIDs and should be considered as first-line pharmacological treatment for knee osteoarthritis, the study authors say. Osteoarthritis affects millions of Canadians.
We spoke with the study's lead author, Dr. Bruno R. da Costa, Acting Director of the Applied Health Research Centre (AHRC) at the Li Ka Shing Knowledge Institute of St. Michael's Hospital, about the findings and why he says opioids should only play a secondary role in osteoarthritis treatment, if at all.
Why is it important to investigate the benefits and harms of different doses of commonly prescribed pharmacological treatments for knee and hip osteoarthritis?
Recent clinical practice guidelines recommend that when these treatments are used, the lowest possible dose should be prescribed to minimize the risk of adverse events. However, it is currently unclear what the lowest but still effective doses of these drugs are. Osteoarthritis affects more than 4.6 million people in Canada. Our findings allow physicians, patients, or their caregivers to have a better understanding of which of these treatments at their lowest doses would be safest while still being effective.
In the larger context of the opioid epidemic, what makes these findings significant?
Although there is robust evidence about the harmful effects of opioids, and international concerns around the opioid epidemic, opioids remain among the most prescribed drugs for osteoarthritis pain in Canada, the United States, the United Kingdom and Australia.
In addition to the immediate reactions following opioid use like nausea, vomiting, and drowsiness, their chronic use is associated with increased risk of fractures, cardiovascular events, opioid dependence, and mortality. Between 2000 and 2017, opioid-related mortality increased by 593 percent in Canada.
In our meta-analysis, none of the opioid interventions, regardless of dose, seemed to have a clinically relevant effect on pain or physical function. Our results show that opioids should only play a secondary role in osteoarthritis treatment. Namely when all other conservative treatment options have been exhausted, if at all.
What surprised you most about the findings?
Even maximum recommended daily doses of opioids do not have an effect in osteoarthritis pain that patients would consider relevant. We did not observe an association between higher opioid doses and greater pain relief
It was also interesting to see that lower doses of topical Diclofenac (Voltaren) have a similar beneficial effect to the most effective oral NSAIDs in knee osteoarthritis. This is important to know as topical NSAIDs would be safer than oral NSAIDs for patients with gastrointestinal or cardiovascular comorbidities, or those who are frail, because of reduced systemic exposure. Adverse events of topical NSAIDs are minimal and mild; most are minor and transient local skin reactions. All topical diclofenac trials included only patients with knee osteoarthritis, so the evidence is unclear for hip osteoarthritis. The depth of the hip joint would make it unlikely for a benefit to occur.
What's next for this research?
We need to better understand the safety of oral NSAIDs in patients with comorbidities, as well as the safety of its long-term use on an as-needed-basis with varying doses, as opposed to fixed daily doses. It would also be helpful to understand if there are sub-groups of patients that have exhausted other conservative treatment options but would still benefit from opioids or acetaminophen.
More information: Bruno R da Costa et al, Effectiveness and safety of non-steroidal anti-inflammatory drugs and opioid treatment for knee and hip osteoarthritis: network meta-analysis, BMJ (2021). DOI: 10.1136/bmj.n2321
Journal information: British Medical Journal (BMJ)
Provided by St. Michael's Hospital