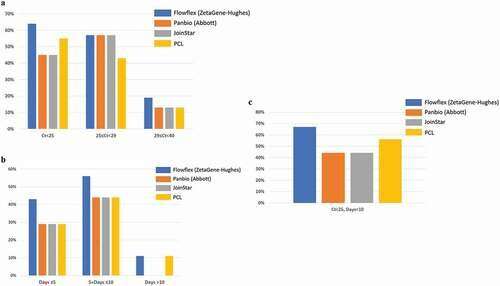
Positive detection rate of SARS-CoV-2 in saliva samples by four SARS-CoV-2 rapid antigen tests: Flowflex (Flowflex SARS-CoV-2 rapid antigen test, ZetaGene-Hughes healthcare, Sweden/UK; blue bars), Panbio (Panbio COVID-19 ag rapid test, Abbott, UK; Orange bars), Joinstar (Joinstar COVID-19 antigen rapid test, China; grey bars), PCL (PCL COVID-19 ag antigen gold saliva lateral flow test, Korea; yellow bars). Saliva specimens were collected from patients with confirmed COVID-19 (n = 44), and 34 samples were above the threshold of detection by RT-PCR (Ct<40). Patients were grouped according to (a) PCR Ct values: Ct<25; 25≤ Ct<29; 29≤ Ct<40; (b) days after COVID-19 symptoms onset: Days≤5; 5< Days≤10; Days≥10; (c) Ct<25, Days<10. Credit: DOI: 10.1080/20008686.2021.1993535
The most common tests for COVID-19 are PCR tests, involving a nose and throat sample taken with a cotton swab. The procedure is often unpleasant, and the tests results require laboratory analysis. In a new study from Lund University in Sweden, researchers have now investigated whether rapid antigen testing can be used on saliva instead of swabbing the nasal cavity. The results are published in Infection Ecology & Epidemiology.
"Although our study isn't definitive, our results indicate that rapid tests using saliva might be good enough for diagnosing COVID-19 in the early phase of infection," says Magnus Rasmussen, specialist in infectious disease medicine at Skåne University Hospital and professor at Lund University, who led the study together with Yang De Marinis, associate professor at Lund University.
Quick diagnostic tools are crucial in reducing the spread of COVID-19. Today, there are several different test methods to identify an ongoing infection. The PCR tests used in healthcare and most commercially available antigen tests are usually taken with swabs in the nasal cavity—a method that many find uncomfortable. Antigen tests are used as a complement to PCR testing when increased test capacity or rapid test results are required. However, there are also saliva tests.
"Saliva-based tests are less unpleasant, simpler and easier to handle. You also do not need trained healthcare staff to spit in a cup," says Magnus Rasmussen.
In the current study, the researchers compared RT-PCR tests with saliva samples they collected from 44 patients. All 44 participants had confirmed COVID-19, and had to clear their throat before spitting. The results showed that coronavirus can be detected in both saliva and nasal cavity samples, but that the concentrations are slightly lower in saliva.
The researchers also examined four different rapid antigen tests available on the market, to see how well they detect the virus in saliva samples.
All four antigen tests were found to be relatively sensitive in detecting the virus early in the infection, as the virus concentration is higher at that point. Later in the infection, when the virus concentration is lower, the antigen tests were not sufficiently sensitive.
"The advantage of a saliva-based rapid test is that you can easily take it at home in peace and quiet. For many, it can make a big difference. If infection occurs in, for example, primary school, the younger unvaccinated students can be screened more quickly with a saliva-based rapid test. For children, it is important that sampling is simple and without discomfort," says Yang de Marinis, who is the first author of the study.
The researchers believe that rapid saliva tests are a good alternative to standard PCR testing, and can also supplement these methods as screening needs increase.
"Before we can start using saliva antigen tests, we need to confirm that they are reliable when identifying COVID-19 in newly infected and previously vaccinated people as well. Such studies are ongoing; within our own research and also elsewhere," concludes Magnus Rasmussen.
More information: Yang De Marinis et al, Detection of SARS-CoV-2 by rapid antigen tests on saliva in hospitalized patients with COVID-19, Infection Ecology & Epidemiology (2021). DOI: 10.1080/20008686.2021.1993535
Provided by Lund University