Customized implants for the rehabilitation of ear malformation
Researchers at the Technion–Israel Institute of Technology and Sheba Medical Center have developed an efficient technology for the fabrication of custom-made functional aesthetic implants for the rehabilitation of congenitally deformed ears.
Microtia is a birth defect that occurs when the external ear fails to develop normally, and as a result, is small and improperly formed. Microtia occurs in 0.1 to 0.3 percent of births. Occasionally, besides the aesthetic issue, microtia also involves hearing loss.
Since the "bones" of the outer ear—the auricle—are in fact flexible cartilage and not bone tissue, the customary technique for microtia reconstruction is to use costal cartilage harvested from the patient's chest. This method involves pain and discomfort as well as risk of further complications. Moreover, constructing an ear that is identical to the other one depends on both the surgeon's creativity and high-level surgical skills.
The journal Biofabrication reports the Israeli researchers' breakthrough, which was achieved through a collaborative project between Professor Shulamit Levenberg of the Faculty of Biomedical Engineering at the Technion and Dr. Shay Izhak Duvdevani, a senior physician in the Otorhinolaryngology Head and Neck Surgery Department and Head of the Tissue Engineering Lab at Sheba Medical Center.
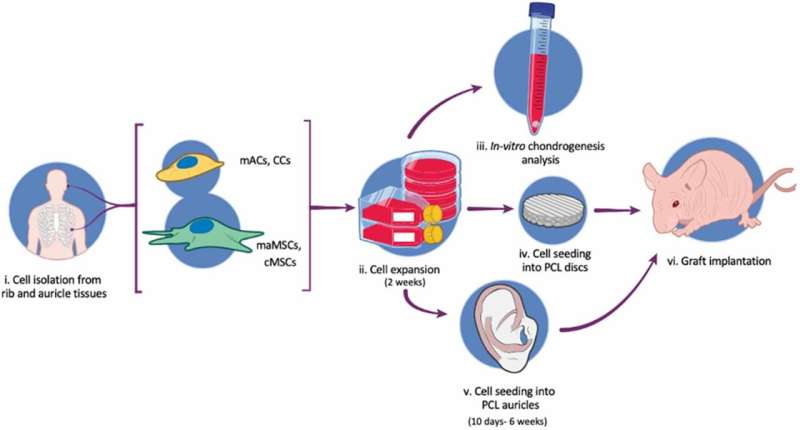
In the current study, the researchers applied new technologies for tissue engineering, developed in Prof. Levenberg's lab under the leadership of Dr. Shira Landau, to fabricate a biodegradable auricle scaffold that formed stable, custom-made neocartilage implants.
The unique scaffold, which allows for the formation of an aesthetic and stable auricle, is 3D-printed and based on a CT scan. It is biodegradable and forms chondrocytes—the cells responsible for cartilage formation—and mesenchymal stem cells. The scaffold has pores of varying sizes, allowing for cell attachment to form stable cartilage.
According to the researchers, engineering an auricle from the patient's own cells will reduce the suffering and risk caused to children as a result of harvesting their costal cartilage. Furthermore, it will allow the surgery to be performed on children as young as six years old, rather than the currently accepted practice of waiting until they are ten. Performing the surgery at a younger age is likely to mitigate the psychological effects of microtia on children.
The researchers monitored cartilage formation within the auricle construct in the lab for between 10 days and six weeks, and then implanted it in a murine model. The outcome: Graft integration was successful, and the prosthetic ear demonstrated good biomechanical function.
Prof. Levenberg says, "One of the challenges in the study was to find a suitable 3D printing method, since fabricating an ear necessitates the use of biodegradable materials that break down in the body without harming it but have an extremely accurate external structure and small pores. We demonstrated all of this in the present research, and estimate that it will be possible to tailor our technology to other applications, such as nasal reconstruction and fabrication of various orthopedic implants."
Dr. Duvdevani says, "In the present study, we achieved a significant breakthrough by means of the integration of medicine and research and collaboration between doctors and researchers. This research is another milestone in the transition to advanced technologies in medicine, where the use of 3D printing and tissue engineering will play a significant part and provide patients with an optimal, state-of-the-art response."
More information: Shira Landau et al, Human-engineered auricular reconstruction (hEAR) by 3D-printed molding with human-derived auricular and costal chondrocytes and adipose-derived mesenchymal stem cells, Biofabrication (2021). DOI: 10.1088/1758-5090/ac3b91




















