Long-term SARS-CoV-2 vaccine responses in older nursing home residents
New research assessing levels of COVID-19 antibodies (against the SARS-CoV-2 spike protein) both before vaccination and at five weeks and six months after nursing home residents received two doses of the Pfizer vaccine provide strong support for the use of vaccine boosters in this cohort.
The research, involving immunologists, geriatricians and nurses from Trinity College Dublin, Tallaght University Hospital (TUH) and several translational research laboratories including Trinity's Trinity Translational Medicine Institute (TTMI) and Trinity Biomedical Sciences Institute (TBSI), has just been published in the Journal of the American Medical Directors Association (JAMDA).
Key results
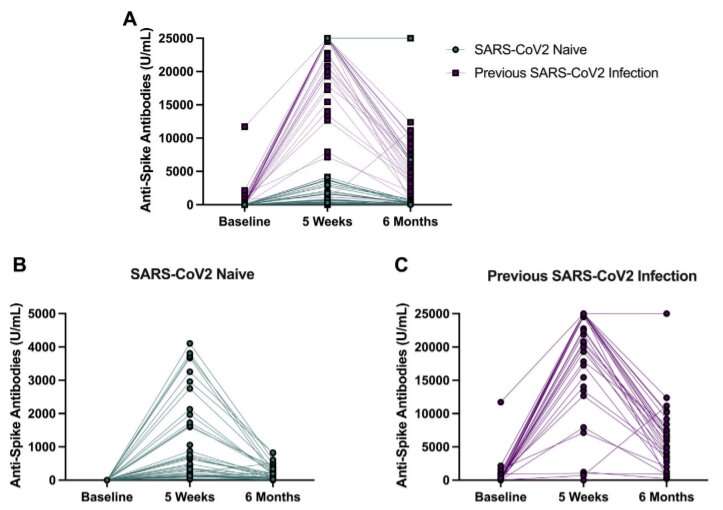
Previous COVID-19 infection, age and degree of frailty (decreased physiological reserve to stressors, which is common in nursing home residents) were all associated with six-month antibody levels post-vaccine. While antibody levels predictably declined over time, this decline was particularly striking in those individuals with no previous evidence of SARS-CoV2 infection.
Further, whereas previous infection was associated with much greater levels of anti-spike antibodies at six months, increasing age and greater levels of frailty were independently associated with lower antibody levels. Importantly, antibody levels were significantly associated with neutralization capacity (the ability of antibodies to neutralize the SARS-CoV-2 virus).
This research highlights the effect of past infection on shaping long-term antibody responses in this group and supports the ongoing use of booster vaccinations in this population. It also suggests that SARS-CoV-2-naïve individuals may be particularly vulnerable.
It is important to note that the study only considered anti-spike antibody levels and did not examine long-term "memory" immune cells and the ability of these to fight off future infection—an area of ongoing research for the group.
Dr. Adam Dyer, specialist registrar in geriatric medicine & Irish clinical academic training fellow in Trinity's School of Medicine and TUH, said:
"Our findings demonstrating lower antibody levels in SARS-CoV-2-naïve individuals and in those with increasing age and frailty tell only part of the story, but they support the ongoing use of vaccine boosters in this vulnerable population."
Professor Sean Kennelly, clinical associate professor in Trinity's School of Medicine, and consultant geriatrician at TUH, said:
"The NH-COVAIR study is an important piece of research that provides support for the use of COVID-19 vaccine boosters in nursing home residents to prevent serious illness. Nursing home residents are frequently excluded from translational research, but as we know they are the population at greatest risk of morbidity and mortality from COVID-19 illness."
More information: Adam H. Dyer et al, Previous SARS-CoV-2 Infection, Age, and Frailty Are Associated With 6-Month Vaccine-Induced Anti-Spike Antibody Titer in Nursing Home Residents, Journal of the American Medical Directors Association (2022). DOI: 10.1016/j.jamda.2021.12.001




















