Third COVID-19 wave hit rural America especially hard
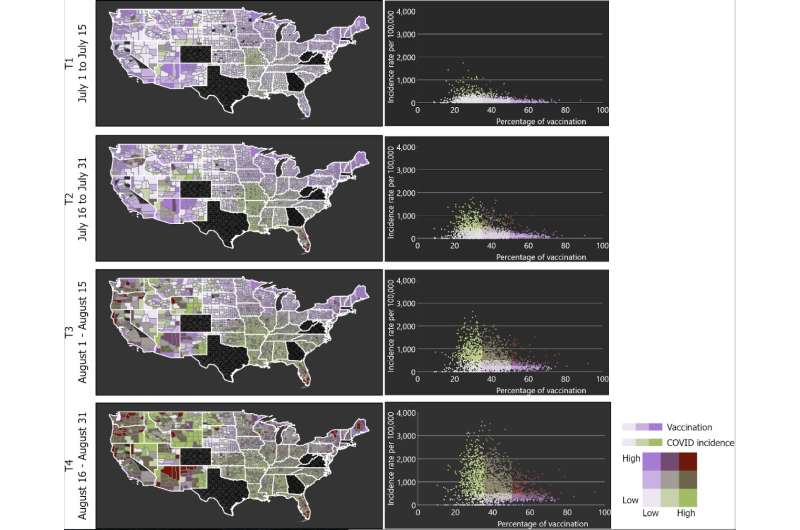
The third wave of the COVID-19 pandemic in the summer of 2021 spread far faster in rural America, much of which has low rates of vaccination.
A new study led by the University of Cincinnati found that rural counties had 2.4 times more infections per 100,000 people than urban areas between July 1 and Aug. 31, 2021, when the delta variant surged across the United States.
About 82% of rural America has a vaccination rate lower than 30%, according to data collected from the Centers for Disease Control and Prevention. Conversely, rural counties accounted for just 131 of the 376 areas with vaccination rates of 50% or more.
Unlike some countries, the United States has a lot of variation in vaccination rates from state to state and county to county. So understanding where vaccinations are lagging could help government and health agencies address vaccine hesitancy and shortfalls in health care, UC epidemiologist and lead author Diego Cuadros said.
He is director of UC's Health Geography and Disease Modeling Lab.
Areas with low vaccination rates experienced a more intense surge of new cases during the third wave of the pandemic in the United States, driven primarily by the delta variant, according to COVID-19 infection data collected by Johns Hopkins University.
The study was published Feb. 10 in the journal JAMA Network Open.
Rural areas in the United States face many challenges responding to the pandemic, including less access to health care compared to urban areas.
"We found that infections from the delta wave increased much faster in low-vaccination areas. Not only did we have more cases per capita in low-vaccination areas but the epidemic infection spread much faster compared to high-vaccination areas," said Cuadros, an assistant professor of geography in UC's College of Arts and Sciences.
"Our study underscores the importance of vaccination to mitigate the rate of spread of COVID-19 in the United States," said study co-author Phillip Coule, MD, associate dean at the Medical College of Georgia at Augusta University.
"Although we have long known that the COVID-19 vaccine is safe and effective, this study concludes that communities with higher vaccination rates have slower rates of community spread when an outbreak of COVID-19 does occur," said Coule, vice president and chief medical officer for Augusta University Health System.
UC's Cuadros said some people have a fundamental misunderstanding of vaccines, which are designed to help the body's immune system fight infection.
"They think it's an invisible shield that protects you against the virus. That's not how it works," Cuadros said.
Vaccinated people can still contract the virus, sometimes called "breakthrough cases," but for most people the vaccinations boost the immune system to prevent catastrophic illness that can lead to hospitalization or death.
Former UC College of Pharmacy Dean Neil MacKinnon, now provost at Augusta University, said knowing which areas have low rates of vaccination can help policymakers and health advocates steer efforts to improve access to health care.
"This tells us something powerful," MacKinnon said. "Rural areas in the United States have faced many challenges responding to the pandemic. Important studies like ours are vital to understanding these areas characterized by vaccination hesitancy and vaccine availability to address concerns in the future."
Now researchers are studying the impact of the omicron variant this winter. Preliminary data, which were not part of the published study, suggest this variant, known for being highly contagious, spread more quickly in congested urban areas. But since far more people per capita in these counties were vaccinated, fewer people in urban areas have died compared to rural areas where vaccinations are lagging.
"Omicron is more infectious than delta and started spreading in highly connected urban areas," Cuadros said. "Most infections are concentrated in high-vaccination areas."
While the latest surge of infection is worse in urban America, omicron is still wreaking havoc on the health of rural America, causing more per capita hospitalizations and deaths there than in urban areas.
"Vaccination still protects you from complications from infection, hospitalization and death," Cuadros said.
Scientists and medical professionals need to do a better job explaining the science to the public to help overcome vaccine hesitancy and restore trust, Cuadros said.
"Science is dynamic. We're always working to develop the best strategies based on what the data tells us," he said.
More information: Diego F. Cuadros et al, Analysis of Vaccination Rates and New COVID-19 Infections by US County, July-August 2021, JAMA Network Open (2022). DOI: 10.1001/jamanetworkopen.2021.47915





















