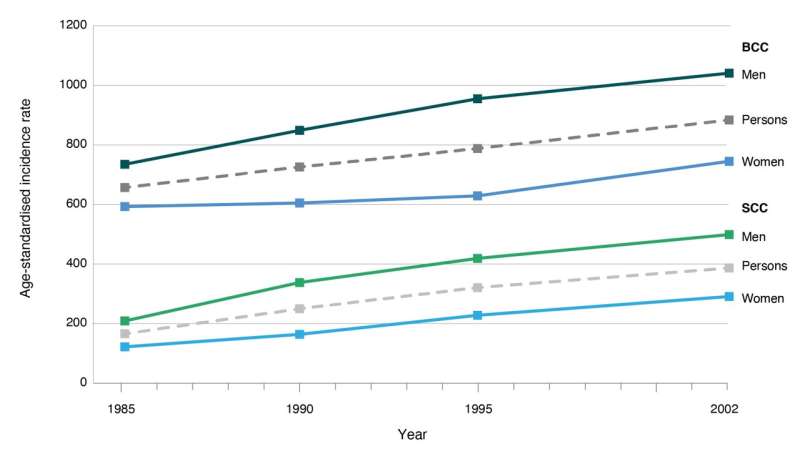
Figure 1. Age-standardized incidence rates (per 100,000) for basal cell carcinoma and squamous cell carcinoma from national surveys conducted in 1985, 1990, 1995 and 2002 BCC = basal cell carcinoma; SCC = squamous cell carcinoma. Note: Rates are standardized to the 1960 world population Sources: National Cancer Control Initiative Skin Cancer Working Group, Staples et al. Credit: Public Health Research & Practice (2022). DOI: 10.17061/phrp3212203
More than two thirds of Australians will be treated for the most common skin cancers in their lifetime, with rates increasing by up to 6% a year over the past three decades, according to new research published today.
The paper, which presents the latest evidence on the incidence of basal cell carcinomas (BCCs) and squamous cell carcinomas (SCCs)—collectively known as keratinocyte cancers—is published in Public Health Research & Practice, a peer-reviewed journal of the Sax Institute.
The authors, led by Associate Professor Catherine Olsen of the QIMR Berghofer Medical Research Institute, calculated the lifetime risk of keratinocyte cancer and trends in treatment rates in Australia, using the latest available data. They found that 69% of Australians (73% of men and 65% of women) will have at least one excision for a histologically confirmed keratinocyte cancer in their lifetime.
Keratinocyte cancers, also known as non-melanoma skin cancers, are the most common cancers in Australia. BCCs grow slowly in the lower levels of the skin's epidermis and make up at least two-thirds of all skin cancers, according to Cancer Council Australia. About one-third of skin cancers are SCCs, which grow rapidly in the upper layer of the epidermis. If left untreated these cancers can damage nerves and nearby tissue and, in the case of SCCs, spread to other parts of the body with potentially lethal consequences. More than 500 Australians die from SCCs every year.
The paper's authors found that not only is the incidence of keratinocyte cancer in Australia very high, it has been increasing over the past three decades, at a rate of between 2 and 6% per year, mostly affecting older age groups.
"This high and increasing burden of skin cancer emphasizes the need for continued investment in skin cancer education and prevention," the authors write.
They say measures to address the growing problem should include support for national mass-media prevention campaigns, a strengthening of regulatory measures to protect children and workers from the harms of overexposure to sunlight and more provision of shade in public spaces.
The authors also note that unlike melanomas, data on keratinocyte cancers is not recorded in state and territory cancer registries, except in Tasmania. They recommend that population-based cancer registries work towards statutory notification and routine reporting of all keratinocyte cancers in Australia to monitor trends.
The paper is published in a special issue of Public Health Research & Practice that focuses on skin cancer prevention and early detection. The issue was supported by and developed in partnership with Cancer Council, Australian Radiation Protection and Nuclear Safety Agency, the Australasian College of Dermatologists and the Australian Skin and the Skin Cancer Research Centre.
Another highlight in this issue is a paper on the early detection and screening of skin cancers. The authors, led by Professor Monika Janda of the University of Queensland, highlight concerns around the current unstructured approach to early detection through opportunistic screening. They discuss new technologies for screening and highlight promising findings from a program to train GPs in the use of dermoscopy.
Other papers examine:
- The lack of national investment in skin cancer prevention in Australia for more than a decade, 40 years on from the iconic 'Slip, Slop, Slap' campaign
- The rising costs of skin cancer, especially for people who develop multiple skin cancers over their lifetime, and for new melanoma therapies
- The need for collaboration to ensure shade is seen as an integral part of healthy built environments to protect Australians from harmful sun exposure
- The wide variation in advice for sun exposure for vitamin D production in Australian and New Zealand guidelines and policies
- The effectiveness, compliance and application of sunscreen for UV protection in Australia.
In an editorial, the issue's guest editors Adjunct Associate Lecturer Paige Preston, Adjunct Associate Professor Craig Sinclair, Associate Professor Catherine Olsen and Professor Anne Cust say that unlike other risk factors for cancer, such as tobacco, alcohol or unhealthy food and drinks, skin cancer has very minimal Australian industry opposition.
"The path to sustained investment is not challenged by industry, but seemingly our own complacency," they write.
"We know what needs to be done—now is the time to do it so that one day Australia is no longer considered the skin cancer capital of the world."
More information: Catherine Olsen et al, Keratinocyte cancer incidence in Australia: a review of population-based incidence trends and estimates of lifetime risk, Public Health Research & Practice (2022). DOI: 10.17061/phrp3212203
Provided by Sax Institute