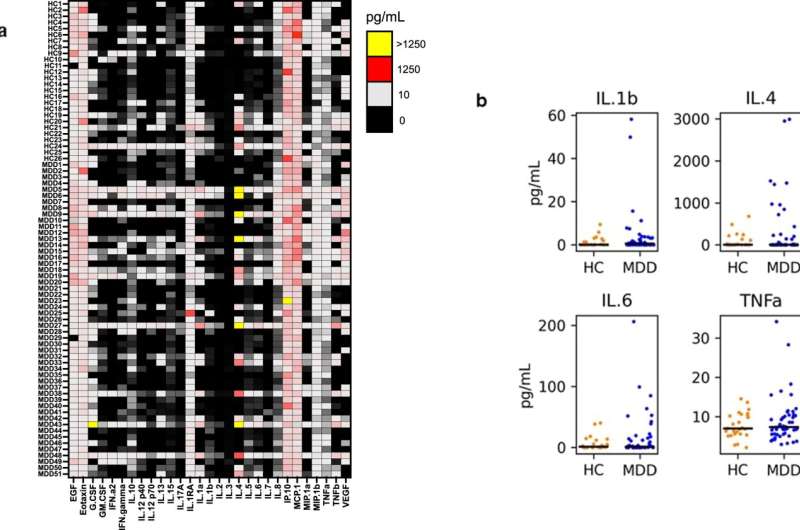
Baseline circulating cytokine profiles in individuals with major depressive disorder (MDD) vs. healthy controls (HC). a Heat map of cytokine profiles. Rows show the data for each individual (subject number, disease grouping), columns show each analyte. Interpolated assay values (picogram/milliliter; pg/mL) are heat mapped, with black denoting the lowest values. EGF epidermal growth factor, G-CSF granulocyte colony-stimulating factor, GM-CSF granulocyte-macrophage colony-stimulating factor, IFN interferon, IL interleukin, IP-10 interferon-gamma induced protein 10 (CXCL10); MCP1 monocyte chemoattractant protein 1, MIP-1α macrophage inflammatory protein 1a (CCL3), MIP-1β macrophage inflammatory protein 1b (CCL4), TNF tumor necrosis factor, VEGF vascular endothelial growth factor. MDD major depressive disorder, HC healthy control. b Comparison of selected cytokine levels in MDD (blue) vs. HC (orange). The black horizontal line denotes median values for each analyte and cohort. The sample size is n = 51 MDD and n = 26 HC. No differences were significant by a Wilcoxon rank-sum test in any of the 29 analytes (all comparisons are shown in Fig. S1, p > 0.1). Credit: Translational Psychiatry (2022). DOI: 10.1038/s41398-022-01883-4
Multiple prior studies have found higher levels of inflammation in older individuals with depression. Now, a new Penn Medicine study has found that clinically depressed older individuals, on average, don't have elevated levels of inflammation if they don't already have other inflammatory conditions such as arthritis.
The new study, published recently in Nature Translational Psychiatry, suggests that depression occurs independently of inflammation for many older adults. Furthermore, depression-inflammation links are due to the greater incidence of inflammatory conditions, which in general are common in older people.
"It is still true that inflammatory illnesses can contribute to depression, but our findings suggest that there is a subset of individuals with late-life depression who do not have elevated levels of inflammation," said study senior author Yvette Sheline, MD, McLure Professor of Psychiatry and Behavioral Research in the Perelman School of Medicine at the University of Pennsylvania.
National surveys in the United States suggest that, although depression is diagnosed more often among younger adults, about five percent of people who are at least 50 years old have had a major depressive episode in the past year. Researchers suspect that many of these cases of late-life depression are caused by inflammation—in part because studies have found higher levels of inflammatory immune proteins in the blood of older people with depression, compared to non-depressed people of the same age.
Prior research also has shown that levels of inflammation markers generally tend to rise with increased age, as chronic illnesses set in and the body's immune-regulating systems weaken. Based on such findings, doctors have tested anti-inflammatory drugs in patients with depression, and have found that they can improve outcomes when added to standard anti-depressant therapy.
The new study reveals, however, that the link between depression and inflammation is not as clear-cut as the prior literature suggests. Sheline and colleagues used online and in-person screening of over 1,100 depressed individuals to recruit a group of 63 individuals, age 50 to 80, who met criteria for major depressive disorder but did not have other inflammatory conditions. Comparing this group to 29 healthy individuals of the same age, even with highly sensitive measurements, the researchers found no significant differences in bloodstream levels of 29 different inflammation-linked immune proteins.
The researchers then randomized 60 of the depressed patients to receive either a standard antidepressant drug, or the antidepressant plus an anti-inflammatory drug, or placebo, for eight weeks. They found that while the two antidepressant-treated groups showed significant improvement in their depression ratings relative to placebo, there was no significant difference in outcome between the antidepressant and the antidepressant-plus-anti-inflammatory group. Moreover, in all three groups, the subjects' blood levels of inflammatory markers were low before treatment and did not drop significantly as a result of treatment. The researchers even tested the cerebrospinal fluid of the subjects for levels of the inflammatory protein IL-1β, and again found low levels both before and after treatment.
The study therefore suggests that, in many older adults, depression occurs independently of inflammation, and probably won't be alleviated by anti-inflammatory treatments unless inflammation is present in addition to depression.
The researchers note, however, that because their study excluded late-life depression patients who have inflammatory disorders, it leaves open the possibility that inflammation from such disorders can contribute to depression.
"Our study supports the view that depression consists of different sub-categories, some with inflammation and some without," said Sheline, who is also director of Penn's Center for Neuromodulation in Depression and Stress. "People who have depression should consult with their doctor to see if they have other illnesses that could cause inflammation, since there is evidence that increased inflammation can cause depressive symptoms."
More information: Eline T. Luning Prak et al, No increase in inflammation in late-life major depression screened to exclude physical illness, Translational Psychiatry (2022). DOI: 10.1038/s41398-022-01883-4
Journal information: Translational Psychiatry