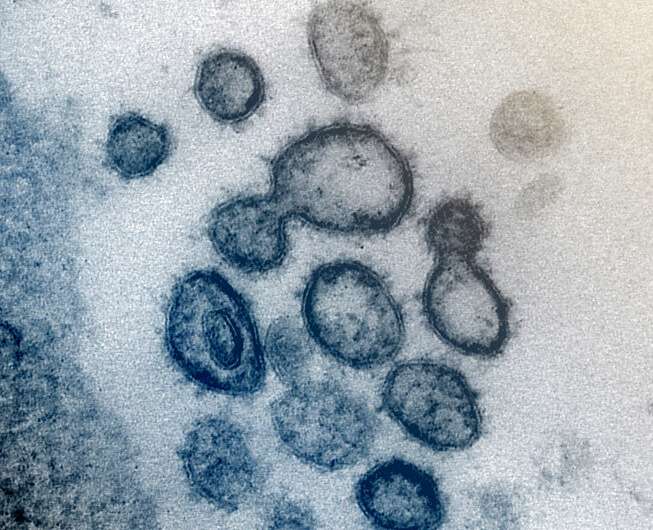
This transmission electron microscope image shows SARS-CoV-2 -- also known as 2019-nCoV, the virus that causes COVID-19 -- isolated from a patient in the US. Virus particles are shown emerging from the surface of cells cultured in the lab. The spikes on the outer edge of the virus particles give coronaviruses their name, crown-like. Credit: NIAID-RML
New research to be presented at this year's European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) in Lisbon, Portugal (23-26 April), suggests that shorter telomeres, a feature of aging, may influence the severity of COVID-19 and the risk of dying from the disease, particularly in women. The study is by Dr. Ana Virseda-Berdices, María Ángeles Jiménez-Sousa and Amanda Fernández-Rodríguez from the Health Institute Carlos III, Madrid, Spain and colleagues.
Telomeres are protective caps on the end of chromosomes (DNA) that shorten over the lifetime, and their length is often used as a measure of cellular age. Shorter telomeres are associated with a number of age-related diseases including cancer and osteoarthritis, and are also linked with higher risk of developing infections. Given the importance of telomere length in cellular health and aging, it is critical to understand the dynamics of telomeres in COVID-19 infection.
In this study, researchers investigated the association between relative telomere length (RTL) at disease onset and COVID-19 mortality in 608 adults hospitalized with COVID-19 during the first wave of the pandemic (from March to September 2020). Blood samples were collected within 20 days of COVID-19 diagnosis or hospitalization, and genetic analysis using polymerase chain reaction (PCR) was done to measure telomere length in blood cells.
Researchers estimated survival probabilities and used modeling to explore the association between RTL and mortality, taking into account patient characteristics including age, gender, smoking status and comorbidities (chronic kidney disease, chronic neurological disease, and neoplasia [abnormal [pre-cancerous] growth cells, tissues in the body]).
Overall, 533 patients survived (average age 67 years, 58% male, 73% white, 24% Hispanic) and 75 died from COVID-19 (average age 78 years, 67% male, 77% white and 21% Hispanic).
The analyses found that in all patients, relative telomere length was significantly inversely associated with dying from COVID-19 at 30 and 90 days after hospital discharge (meaning shorter telomeres were associated with an increased risk of death, or longer telomeres were associated with a reduced risk of death).
Further analyses stratifying by age and gender, revealed that a longer RTL was associated with a 70% lower risk of dying from COVID-19 in all women at 30 days, and a 76% reduced risk of dying from the disease at 90 days.
Similarly, in women aged 65 years or older, longer RTL was associated with a 78% lower risk of death from COVID-19 at 30 days, and 81% reduced risk at 90 days.
However, no significant differences were found in relative telomere length between men who survived COVID-19 and those who died of the disease.
"Our findings implicate telomere length in COVID-19 mortality and highlight its potential as a predictor of death and severe outcome, particularly in older women" says Dr. Virseda Berdices. "While we do not know the reasons for the strong association found in women, it's possible that the lack of association between telomere length and COVID-19 mortality in men could be due to increased comorbidities and risk factors in men that masked the effect. Female patients tend to present with less severe disease and are more likely to survive COVID-19, probably due to fewer lifestyle risk factors and comorbidities than men. Besides aging, telomere dysfunction is also associated with smoking, poor diet, higher body mass index and other factors that promote oxidative stress, chronic inflammation and cancer."
The authors acknowledge that the study was observational and does not prove cause and effect, and was conducted during the first wave of the pandemic, which may limit the conclusions that can be drawn.
Provided by European Society of Clinical Microbiology and Infectious Diseases