Antibiotics can lead to fungal infection because of disruption to the gut's immune system
Patients prescribed antibiotics in hospital are more likely to get fungal infections because of disruption to the immune system in the gut, according to a new study from the University of Birmingham and National Institutes of Health.
Using immune-boosting drugs alongside the antibiotics could reduce the health risks from these complex infections say the researchers.
The life-threatening fungal infection invasive candidiasis is a major complication for hospitalized patients who are given antibiotics to prevent sepsis and other bacterial infections that spread quickly around hospitals (such as C. diff). Fungal infections can be more difficult to treat than bacterial infections, but the underlying factors causing these infections are not well understood.
A team in the University's Institute of Immunology and Immunotherapy, in conjunction with researchers at the National Institutes of Health, discovered that antibiotics disrupt the immune system in the intestines, meaning that fungal infections were poorly controlled in that area. Unexpectedly, the team also found that where fungal infections developed, gut bacteria were also able to escape, leading to the additional risk of bacterial infection.
The study, published in Cell Host and Microbe, demonstrates the potential for immune-boosting drugs, but the researchers also say their work also highlights how antibiotics can have additional effects on our bodies that affect how we fight infection and disease. This in turn underscores the importance of careful stewardship of available antibiotics.
Lead author Dr. Rebecca Drummond said: "We knew that antibiotics make fungal infections worse, but the discovery that bacterial co-infections can also develop through these interactions in the gut was surprising. These factors can add up to a complicated clinical situation—and by understanding these underlying causes, doctors will be better able to treat these patients effectively."
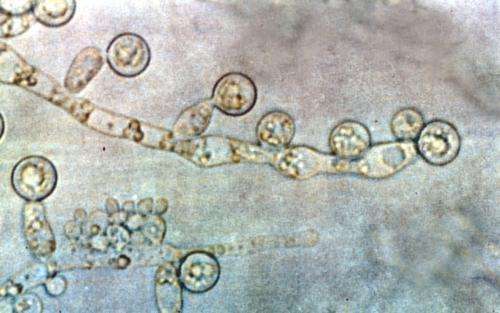
In the study, the team used mice treated with a broad-spectrum antibiotic cocktail and then infected these animals with Candida albicans, the most common fungus that causes invasive candidiasis in humans. They found that although infected mice had increased mortality, this was caused by infection in the intestine, rather than in the kidneys or other organs.
In a further step, the team pinpointed what parts of the immune system were missing from the gut after antibiotic treatment, and then added these back into the mice using immune-boosting drugs similar to those used in humans. They found this approach helped reduce the severity of the fungal infection.
The researchers followed up the experiment by studying hospital records, where they were able to show that similar co-infections might occur in humans after they have been treated with antibiotics.
"These findings demonstrate the possible consequences of using antibiotics in patients who are at risk of developing fungal infections," added Dr. Drummond. "If we limit or change how we prescribe antibiotics we can help reduce the number of people who become very ill from these additional infections—as well as tackling the huge and growing problem of antibiotic resistance."
More information: Long-term Antibiotics Promote Mortality After Systemic Fungal Infection by Driving Lymphocyte Dysfunction and Systemic Escape of Commensal Bacteria, Cell Host & Microbe (2022). dx.doi.org/10.1016/j.chom.2022.04.013


















