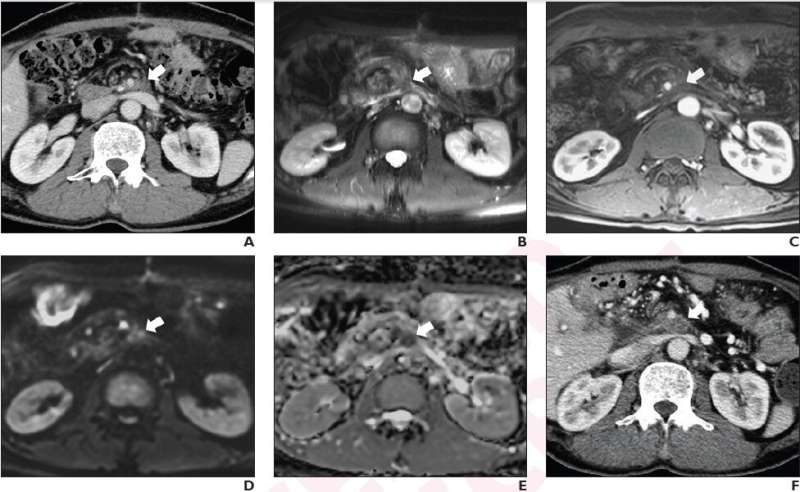
A. Axial contrast-enhanced CT image shows 1.7 cm lesion (arrow) with ill-defined margin at left side of superior mesenteric artery. B. On axial T2-weighted image, mass is hyperintense to paravertebral muscle (arrow). C. On arterial phase post-contrast T1-weighted image, mass shows mild enhancement (arrow) compared to unenhanced image; enhancement pattern classified as early. D. On DWI with b-value of 800 mm2/s, mass is hyperintense (arrow) to paravertebral muscle. E. On ADC map, mass is visually hypointense (arrow) to paravertebral muscle. Findings indicate presence of qualitative diffusion restriction; lesion ADC value was 0.96 × 10−3 mm2/s. F. Axial image from CT performed 6 months after MRI shows increase in lesion's greatest axial diameter by more than 5 mm (arrow), indicating soft tissue abnormality represents locally recurrent tumor. Credit: American Roentgen Ray Society (ARRS), American Journal of Roentgenology (AJR)
According to ARRS' American Journal of Roentgenology (AJR), adding diffusion-weighted MRI (DWI) to conventional MRI improves the differentiation of locally recurrent tumor and post-surgical fibrosis after pancreatic ductal adenocarcinoma (PDAC) resection, primarily due to improved sensitivity for recurrence.
"The findings indicate a potential role for MRI with DWI in surveillance protocols after PDAC resection," clarified corresponding author Tae Wook Kang, MD from Samsung Medical Center in Seoul, South Korea.
Kang and colleagues' retrospective study included 66 patients (35 men, 31 women; mean age, 60.5 years) with PDAC resection between January 2009 and March 2016, who underwent postoperative surveillance CT demonstrating a soft tissue lesion at the operative site or at the site of peripancreatic vessels and subsequent MRI with DWI for further evaluation. CT at least 6 months after MRI served as reference standard, with increase in size of the soft tissue by ≥5 mm differentiating locally recurrent tumor (n=26) and post-surgical fibrosis (n=40). Two observers independently reviewed MRI examinations in separate sessions: conventional MRI alone vs MRI with DWI.
Compared with MRI alone, MRI and DWI showed higher sensitivity (observer 1: 88.5% vs 61.5%, p=.008; observer 2: 84.6% vs 42.3%, p= .001) without difference in specificity (observer 1: 72.5% vs 80.0%, p=.08; observer 2, 95.0% vs 85.0%, p=.10) in detecting local recurrence after PDAC resection.
"MRI with DWI as a problem-solving tool during post-operative surveillance after PDAC resection could facilitate earlier detection of recurrences," the authors of this AJR article added, "guiding prognostic assessment and treatment decisions."
More information: Nari Shin et al, Utility of Diffusion-Weighted MRI for Detection of Locally Recurrent Pancreatic Cancer After Surgical Resection, American Journal of Roentgenology (2022). DOI: 10.2214/AJR.22.27739
Journal information: American Journal of Roentgenology
Provided by American Roentgen Ray Society