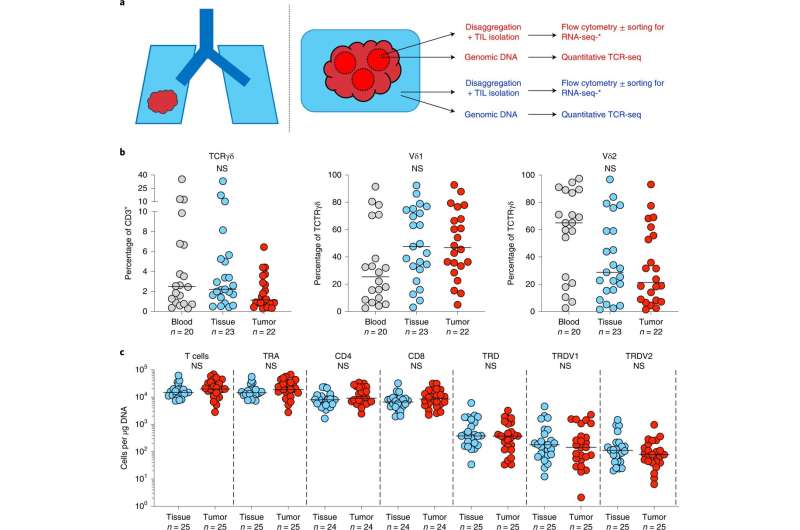
Experimental design and γδ T cell composition in lung tissues and NSCLCs. a, Overview of study design. Paired tumor regions (red) and NT lung tissues (blue) collected under the TRACERx Study were enzymatically digested to extract tissue/TILs. TILs were cryopreserved and thawed at a later date for flow cytometry ± RNA-seq. In parallel, gDNA was extracted from undigested matched tumor regions and NT lung tissues and sent for subsequent quantitative TCR-seq. In addition, PBMCs were isolated from contemporaneous blood draws and cryopreserved before subsequent thaw for flow cytometry. b, Percentage of CD3+ T cells staining for TCRγδ (left) and percentage of TCRγδ T cells staining for Vδ1 (middle) and Vδ2 (right) in PBMCs (blood), NT lung tissues (tissue) and tumors (tumor). Not all patients had paired samples. The bar represents the median. The Kruskal–Wallis test with post-hoc Dunn's test corrected for multiple testing was used. c, Absolute counts of total T cells, αβ T cells (TRA), γδ T cells (TRD) and Vδ1 (TRDV1) and Vδ2 (TRDV2) T cells per microgram of DNA determined by TCR-seq. Absolute counts of CD4+ αβ T cells (CD4) and CD8+ αβ T cells (CD8) were determined by mapping the proportion of CD3+/TCRγδ− T cells staining for CD4 or CD8 in flow cytometry analysis of paired TILs. No significant differences were observed within demarcated T cell subsets between NT tissues and tumors. Samples with <1 cell μg−1 of DNA were not plotted for the purposes of visualization. The bar represents the median. A two-tailed Mann–Whitney U-test was used within demarcated T cell subsets. Significant P values are shown. NS, not significant. The n numbers and datapoints represent independent patients. Credit: Nature Cancer (2022). DOI: 10.1038/s43018-022-00376-z
Around 48,500 people are diagnosed with lung cancer in the UK each year. New treatments are desperately needed as fewer than 20% of patients survive for five years after diagnosis, and it is the biggest cause of death from cancer.
In their study published in Nature Cancer today, scientists from King's, the Francis Crick Institute and UCL investigated the role of specialist immune cells, called gamma delta (γδ) T cells, in lung cancer.
γδ T cells are distinct from more the abundant "conventional" T cells that are most often implicated in fighting cancer. These cells are unique in that they are present at high levels in the tissues from which cancers develop and in their ability to respond to "stress" signals that almost all cancer cells express. In previous laboratory experiments, researchers have shown that once activated by stress signals, these immune cells can kill cancerous cells in a petri dish. This means they are theoretically well-placed to detect and protect against developing tumors.
As part of the TRACERx study, the team analyzed samples of lung tumors and non-cancerous lung tissue from 25 patients with non-small-cell lung cancer. They found that a subtype of γδ T cells, Vδ1 cells, were present in both tumors and non-cancerous lung tissue.
Their presence within the tumor was associated with remaining cancer-free after surgery (remission). But intriguingly, their presence in non-cancerous tissue was a stronger predictor of ongoing remission, suggesting that these cells continue to stand guard against cancer even after removal of the tumor.
The team also demonstrated that these cells make the right molecules to kill tumor cells within the tumor itself, something that had only been demonstrated before in artificial conditions. They found that Vδ1 T cells had stem-like features that may enable them to self-replenish within tumors, a property which is important for long-lived tumor control.
The researchers further checked the impact of these cells on lung cancer survival by analyzing data from around 800 non-small-cell lung tumors contained in The Cancer Genome Atlas, a large public database. They used expression of a particular gene as an indicator of Vδ1 T cell levels and determined that people who had high levels of these cells in their lung tumor were more likely to survive. They also analyzed data from the INSPIRE clinical trial showing that patients with more Vδ1 T cells within various solid tumors were more likely to respond to the immunotherapy treatment pembrolizumab.
"It's less than three years since we showed that people with high levels of Vδ1 in their breast tumor were more likely remain disease-free. We've now also uncovered their important role in lung cancer, on the heels of other studies implicating their importance in ovarian cancer," say Professor Adrian Hayday, from The School of Immunology & Microbial Sciences
He added that "while more research is needed to understand and harness the anti-cancer properties of these cells, this work is a positive development for oncologists considering how the cells might best be applied in both the prognosis and treatment of many different patients."
Charlie Swanton, co-senior author, group leader at the Crick and UCL and Chief Investigator of TRACERx and Chief Clinician at Cancer Research UK, says, "Immunotherapies are important tools for treating cancer, however sadly in the case of lung cancers they often do not work for a long period and it is hard for doctors to predict which patients will benefit from these treatments. This work adds to the body of evidence of the importance of T cells, in this case Vδ1's, in protection from disease relapse after surgery.
"By better understanding how gamma delta T cells and the wider immune system works in the face of cancer and in response to treatments, we hope to uncover potential new ways to tackle the disease and offer more hope to patients."
The team also uncovered important findings about the nature and biology of these unique immune cells in human lungs that may have additional implications for future patient care. They found that of the two major γδ T cell subtypes, Vδ1 T cells are more widely present in the lung than Vδ2 T cells which are more prevalent in the blood. And only Vδ1 T cells were a good indicator of survival.
Yin Wu, lead author, Wellcome Trust Clinical Research Career Development Fellow, and honorary consultant medical oncologist, says, "This understanding could help explain why previous clinical trials using γδ T cells to treat lung cancers have not been very successful, as these have used therapies derived from the Vδ2 subset."
Gamma delta T cell therapies are already being used in early-stage clinical trials for patients with blood cancer. Gamma Delta Therapeutics, a company co-founded by Adrian Hayday, aims to harness the activity of these cells to develop "off-the-shelf" cell therapies for a broad range of cancers and auto-inflammatory diseases.
More information: Yin Wu et al, A local human Vδ1 T cell population is associated with survival in nonsmall-cell lung cancer, Nature Cancer (2022). DOI: 10.1038/s43018-022-00376-z
Journal information: Nature Cancer
Provided by King's College London