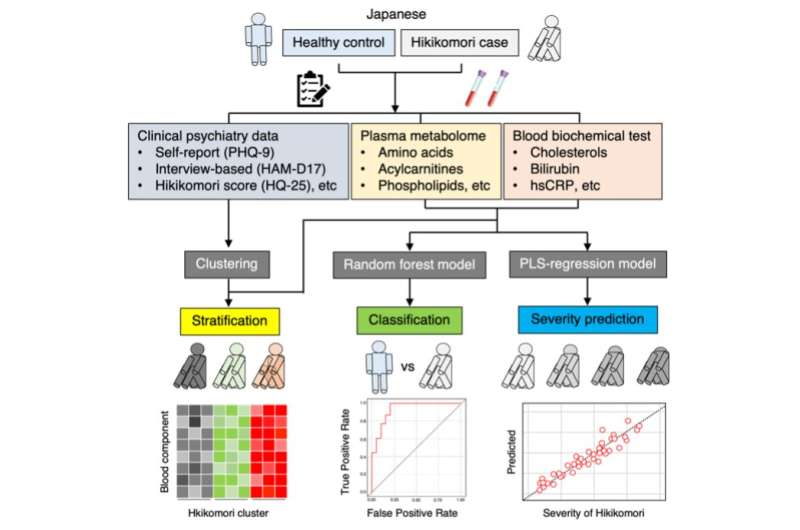
Researchers from Kyushu University used blood metabolome and clinical data to clarify the components characteristic to hikikomori, and machine learning models were created for the classification, prediction of the severity, and stratification of hikikomori.
Researchers at Kyushu University have identified a number of key blood biomarkers for pathological social withdrawal, known as hikikomori. Based on their findings, the team was able to distinguish between healthy individuals and hikikomori patients as well as determine the severity of the condition.
According to Japan's Ministry of Health, Labour, and Welfare, hikikomori is a condition in which individuals do not to leave their dwelling and isolate themselves away from society and family for a period exceeding six months. Also identified as "pathological social withdrawal," hikikomori is estimated to afflict more than one million people in Japan today. While it has been historically identified as a Japanese culture-bound syndrome, evidence over the last few decades has shown that it is becoming a global phenomenon, with some fearing the COVID-19 pandemic catalyzing a global wave of hikikomori patients.
In 2013, the Kyushu University Hospital established the world's first outpatient clinic for hikikomori research in hopes of developing support systems for patients through biological, psychological, and social understanding of the condition.
In a report published in Dialogues in Clinical Neuroscience, lead researcher Takahiro A. Kato of Kyushu University's Faculty of Medical Sciences explains that while the sociological underpinnings of the condition are carefully studied, major gaps remain in the understanding of the biological aspects of hikikomori.
"Mental illnesses such as depression, schizophrenia, and social anxiety disorder are occasionally observed in hikikomori individuals. However, our past research shows that it is not that simple, and that it is a complex condition with overlaps of different psychiatric and non-psychiatric elements," explains Kato. "Understanding what happens biologically will help us greatly in identifying and treating hikikomori."
The team conducted blood biochemical tests and collected data on the plasma metabolome—small molecules found in blood such as sugars, amino acids, and proteins—from 42 unmedicated hikikomori individuals and compared it with data from 41 healthy volunteers. In total, data for 127 molecules were analyzed.
"Some of our key findings showed that, in the blood of men with hikikomori, ornithine levels and serum arginase activity were higher while bilirubin and arginine levels were lower," states first author of the paper Daiki Setoyama. "In both men and women patients, long-chain acylcarnitine levels were higher. Moreover, when this data was further analyzed and categorized, we were able to distinguish between healthy and hikikomori individuals, and even predict its severity."
Ornithine is an amino acid produced from the amino acid arginine with the help of the enzyme arginase. These molecules are vital in many bodily functions, including blood pressure regulation and the urea cycle.
Bilirubin is made when the liver breaks down red blood cells and is often used as a marker for proper liver function. Patients with major depression and seasonal affective disorder have been reported to have lower blood bilirubin levels.
Finally, acylcarnitines play an important role in supplying energy to the brain. Its levels decrease when patients with depression take selective serotonin reuptake inhibitors. However, patients with hikikomori differ from patients with depression in that only the long-chain acylcarnitines are elevated in hikikomori whereas short-chain acylcarnitines remain the same.
Says Kato, "Identifying the biomarkers of hikikomori is the first step in uncovering the biological roots of the condition and connecting them to its severity. We hope these findings will lead to better specialized treatments and support for hikikomori."
"Many questions remain, including understanding the root causes behind these biomarkers. Today, hikikomori is spreading worldwide, thus, we must conduct international investigations to understand the similarities and differences between patients with hikikomori globally," he concludes.
More information: Daiki Setoyama et al, Blood metabolic signatures of hikikomori, pathological social withdrawal, Dialogues in Clinical Neuroscience (2022). DOI: 10.1080/19585969.2022.2046978
Provided by Kyushu University