New blood biomarker identified for status of fatty liver disease
A MedUni Vienna study team has identified the role of a specific subtype of macrophages (white blood cells) in progressive non-alcoholic fatty liver disease. As part of the immune system, these cells have a protective function against fibrosis and liver cirrhosis. At the same time, they are useful as biomarkers of liver disease progression as they can be measured by a blood test. The results were recently published in the Journal of Hepatology.
Non-alcoholic fatty liver disease (NAFLD) is one of the most common chronic liver diseases worldwide and is estimated to affect about 30% of the European population. Chronic non-alcoholic fatty liver disease can develop into irreversible liver cirrhosis, which can only be cured by liver transplantation. Therefore, it is particularly important to identify patients with non-alcoholic fatty liver disease early on.
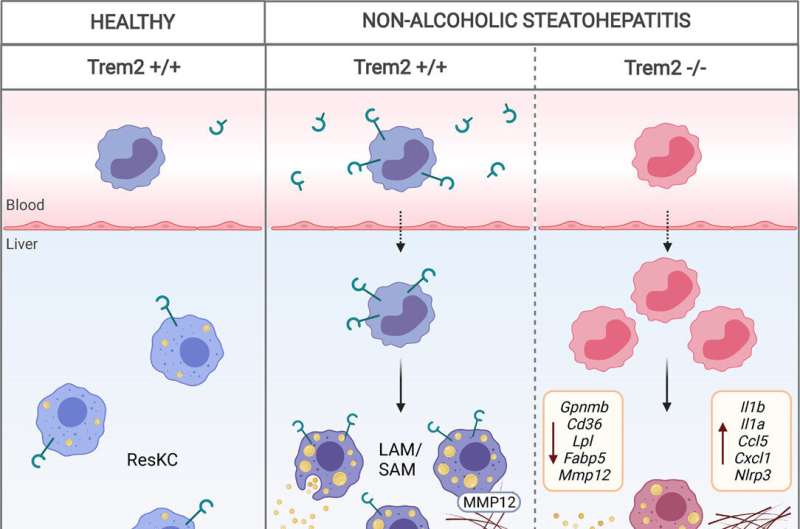
The pathogenesis (development) of non-alcoholic fatty liver disease, especially advanced steatohepatitis (NASH, also: non-alcoholic fatty liver hepatitis), is associated with profound changes in immune cells in the liver. Recently, the increased accumulation of a subtype of macrophages that express high levels of the receptor TREM2 has been described in fatty liver disease.
However, the role of TREM2-positive macrophages in non-alcoholic fatty liver disease was hitherto unknown. The MedUni Vienna research team led by Christoph Binder and Tim Hendrikx from the Department of Laboratory Medicine was able to show in an animal model that these specific macrophages have a protective function in fibrosis—a precursor to liver cirrhosis. These cells are found in greater numbers in the affected areas of the liver upon non-alcoholic fatty liver disease-associated liver inflammation, where they accumulate particularly in areas of cellular damage and fibrosis.
The interdisciplinary study team also demonstrated in bone marrow transplantation models that hematopoietic TREM2 deficiency prevents efficient fat storage and breakdown of excess connective tissue (extracellular matrix), leading to increased steatohepatitis, cell death and fibrosis. Hence, TREM2-positive macrophages fulfill an important protective function in non-alcoholic fatty liver disease, where they prevent fat accumulation, inflammatory processes and progression of the disease to liver fibrosis. "It may be possible to develop new therapeutic approaches to treat fatty liver hepatitis by enhancing this protective function of TREM2-positive macrophages," said Florentina Porsch, co-first author of the study.
TREM2 exists both as a membrane receptor on cells as well as as a soluble form (sTREM2) that is detectable in blood. The role of this soluble form in the immune system is not yet clear. However, the study authors discovered that it is useful in patients for determining the current status of the disease and helps to distinguish between the different stages of fatty liver hepatitis much better than previously known biomarkers used in clinical practice. "The soluble form of TREM2 is an excellent biomarker for identifying and staging advanced liver disease, which can progress from fatty liver disease to incurable cirrhosis if left untreated," explains first author Tim Hendrikx from MedUni Vienna's Department of Laboratory Medicine.
More information: Tim Hendrikx et al, Soluble TREM2 levels reflect the recruitment and expansion of TREM2+ macrophages that localize to fibrotic areas and limit NASH, Journal of Hepatology (2022). DOI: 10.1016/j.jhep.2022.06.004



















