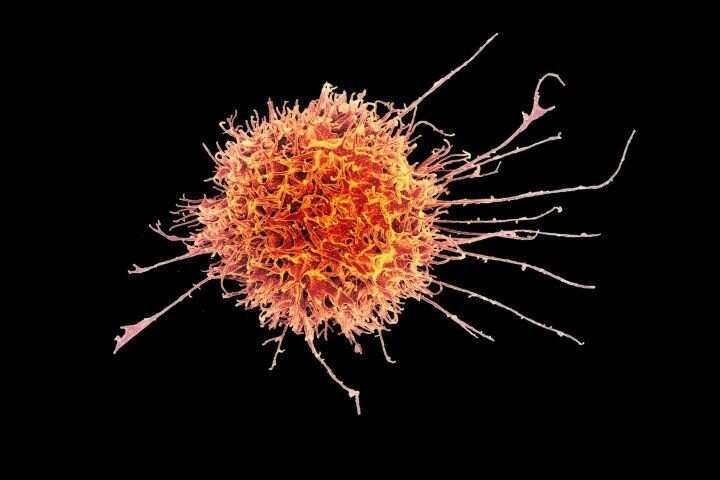
Colorized scanning electron micrograph of a natural killer cell from a human donor. Credit: National Institutes of Allergy and Infectious Diseases
Scientists have identified a new treatment combination that is highly effective at suppressing the growth of head and neck tumors.
A new study led by a team of scientists at the Institute of Cancer Research, London, in mice, showed that a combination of radiotherapy, a drug that inhibits DNA damage repair and an immunotherapy can activate natural killer (NK) cells—a type of white blood cell with the ability to kill cancer cells directly.
Head and neck cancers develop in the mucous membranes of the mouth, nose and throat, and nearly 750,000 new cases are diagnosed globally every year. Treatments include surgery, radiotherapy, chemotherapy and immunotherapy, but patients whose disease progresses after attempting these treatments have limited options.
Only around 15–20% of patients with head and neck cancer respond to current immunotherapies. However, the novel NK cell-targeting strategy described in this study could considerably expand the number of patients with these cancers who benefit from immunotherapy.
Enhancing the effects of radiotherapy
Radiotherapy kills cancer cells by causing DNA damage, which in normal cells is repaired through proteins from DNA damage repair pathways. Many cancer cells have lost important DNA repair functions and therefore rely heavily on a few remaining repair pathways to survive.
One key protein involved in DNA damage repair is called ataxia telangiectasia and Rad3-related protein (ATR). Previous studies have shown that using ATR inhibitors in combination with radiotherapy leads to an influx of immune cells to the tumor site, resulting in better antitumor responses in mice. This combination therapy is currently being investigated in clinical trials.
Targeting natural killer cells
In this new study, published in the Journal for ImmunoTherapy of Cancer, the researchers showed that mice receiving radiotherapy plus an ATR inhibitor drug had delayed tumor growth and survived longer than mice receiving either treatment alone.
The researchers found that the combination therapy led to more NK cells in the tumor microenvironment—the area immediately around the tumor—increased expression of genes associated with their activity, and more inflammation. These events did not occur when NK cells were selectively removed from the site.
'Killer' combination
The team noticed that in response to the combination therapy, activated NK cells and tumor cells displayed new immune checkpoint proteins—the "brakes" of the immune system—on their cell surfaces. This raised the intriguing question of whether these proteins could be potential therapeutic targets.
The researchers then discovered that they could significantly boost the antitumor activity of the NK cells by adding drugs that blocked two of these specific immune checkpoint proteins, called TIGIT and PD-1, following radiotherapy plus ATR inhibitor treatment. This new approach was even more effective at delaying tumor growth and prolonging survival in mice.
Strikingly, some mice treated with the new combination for head and neck cancer showed complete tumor eradication.
Translating it to the clinic
Advantageously, the researchers were also able to access blood samples from patients with advanced cancer undergoing palliative radiotherapy and ATR inhibitor treatment in the Phase I PATRIOT trial to analyze them and determine if the findings may apply to humans.
The samples revealed similar changes in NK cells and immune checkpoint proteins as seen in the mouse studies, supporting the rationale for adding immunotherapy to radiotherapy plus ATR inhibitor treatment in future clinical trials.
Study first author Emmanuel Patin, Postdoctoral Training Fellow in the Targeted Therapy Team at the ICR said:
"In our study, we revealed an important role for natural killer cells during the tumor immune response and the potential to harness them as part of future therapy. This is the first time a combination of this type has been used to target NK cells as a means of triggering tumor eradication—and our new strategy could lead to a great alternative to traditional approaches, allowing more patients to benefit from immunotherapy."
Study leader Professor Kevin Harrington, Head of the Division of Radiotherapy and Imaging at the ICR, and Consultant Oncologist at The Royal Marsden NHS Foundation Trust, said:
"Our study combined radiation treatment with a drug that enhanced its effects, in this case a DNA repair inhibitor, to activate the immune system against a cancer target in mice. We then fine-tuned the immune response that occurred using specific immune checkpoint inhibitors.
"The exciting thing is that we can design completely new ways to treat patients with head and neck cancers and other radiocurable diseases by combining completely novel targeted drug combination strategies, like this one.
"We hope that our work will lead to further evaluation of this approach with other immune checkpoint models and, potentially, be included in part of the ongoing ADePT-DDR trial, which is evaluating ATR inhibitor and radiotherapy with or without immunotherapy in patients with head and neck cancer."
More information: Emmanuel C Patin et al, Harnessing radiotherapy-induced NK-cell activity by combining DNA damage–response inhibition and immune checkpoint blockade, Journal for ImmunoTherapy of Cancer (2022). DOI: 10.1136/jitc-2021-004306
Provided by Institute of Cancer Research