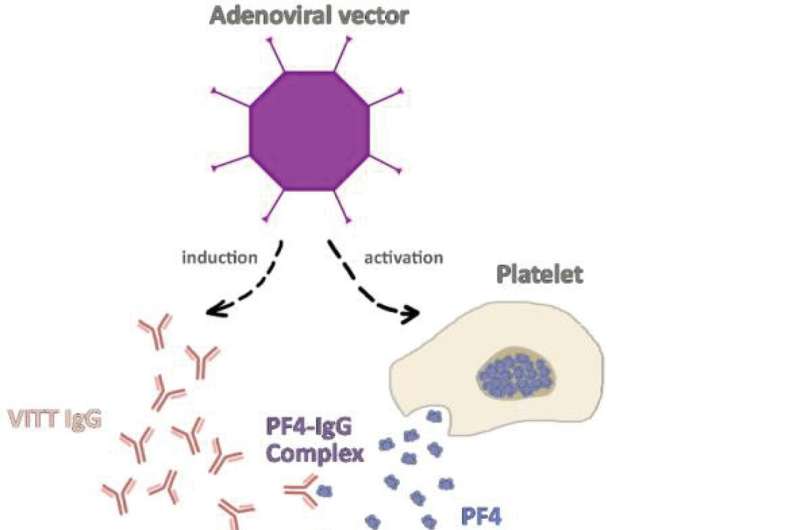
The pathogenesis of vaccine-induced immune thrombotic thrombocytopenia (VITT). Vector-based COVID-19 vaccines, particularly ChAdOx1 COVID-19 vaccine was shown to induce platelet activation alongside platelet factor 4 (PF4) autoantibodies formation. The activated platelets secret greater amount of PF4 which binds to autoantibodies forming the PF4-IgG complex. As a result, FcγRIIA receptor mediated platelet activation leads to widespread thrombosis and secondary thrombocytopenia. Credit: Frontiers in Immunology (2022). DOI: 10.3389/fimmu.2022.872683
As fear of vaccine related adverse events is one of the main reasons for vaccine hesitancy, the authors of a new study published today in Frontiers in Immunology reviewed recent medical literature to see how often adverse events following immunization (AEFIs) occur.
The researchers, who focused on three COVID-19 vaccines—Pfizer, Moderna and AstraZeneca—found AEFIs are rare and, when they do occur, are usually non-life-threatening.
"We embarked on the review to help alleviate public concern about adverse events following immunization, increase the public's willingness to be vaccinated and to guide physicians in rapidly identifying them," says Dr. Nicola Bragazzi, a Postdoctoral Fellow at York's Faculty of Science and the study's corresponding author.
Autoimmune AEFIs of the three COVID-19 vaccines include neurological ones, such as Guillain-Barre syndrome (GBS), transverse myelitis, Bell's palsy, and myocarditis, as well as the more recent concern of vaccine-induced immune thrombotic thrombocytopenia/vaccine-induced prothrombotic immune thrombotic thrombocytopenia (VITT/VIPITT).
Bell's palsy and myocarditis are seemingly the greatest risk when it comes to the mRNA-based COVID-19 vaccines, however, in addition to their rarity, the disease course is mild and full recovery is the rule. In addition, GBS and VITT/VIPITT were found to be associated mainly with the adenovirus vector based COVID-19 vaccines, still with a low rate.
Overall, the study found that the rate of occurrence is either very low, similar to the occurrence rate in the general population or even much lower in comparison to the COVID-19 infection itself.
More information: Naim Mahroum et al, COVID-19 Vaccination and the Rate of Immune and Autoimmune Adverse Events Following Immunization: Insights From a Narrative Literature Review, Frontiers in Immunology (2022). DOI: 10.3389/fimmu.2022.872683
Journal information: Frontiers in Immunology
Provided by York University