Researchers use mathematical modeling to explain immunotherapy responses
Immunotherapies that activate the immune system to seek and kill cancer cells have greatly improved outcomes for many patients with solid tumors. There is still, however, a subset of patients who do not see benefit from this type of therapy. Currently, there are no immune biomarkers that explain how patients with similar disease and patient characteristics can have different outcomes. In a new article published in the Journal for ImmunoTherapy of Cancer, Moffitt Cancer Center researchers demonstrate how mathematical modeling can be used to analyze the impact of different cancer treatments on tumor and immune cell dynamics and help predict outcomes to therapy and personalize cancer treatment.
It is known that interactions between cancer cell populations with the surrounding immune environment impact the development and progression of cancer and patient responses to immunotherapy. Some patients respond well to immunotherapies, while other patients do not. However, it is unclear what differentiates these patients.
"Just like early stage cancers are treated differently than late-stage disease, tumors with different degrees of immune involvement may need very different therapeutic approaches," said Rebecca Bekker, article first author and Cancer Biology Ph.D. student at Moffitt.
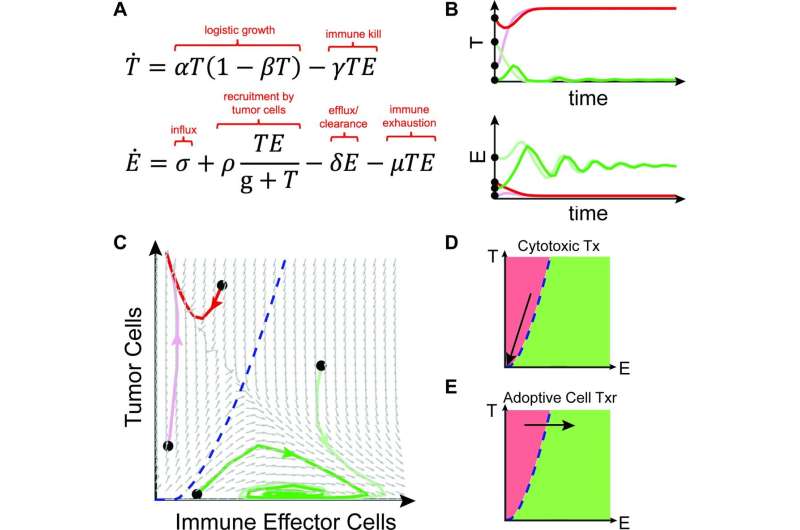
Moffitt researchers wanted to improve their understanding of tumor and immune cell interactions to help predict outcomes for patients and identify the best therapeutic options. Knowing these dynamics are extremely complex and difficult to study in a laboratory setting, the team used an alternative approach to conceptualize these interactions with mathematical modeling. They developed a model that simulates interactions between all possible combinations of tumor cell and immune cell population numbers over time. They included parameters for the rate of tumor cell growth and elimination, and immune cell recruitment and exhaustion. The outcomes of their model were either immune escape, wherein the tumor cells grew to their maximum potential, or tumor control through the antitumor activity of immune cells.
The researchers then used their model to simulate and predict outcomes to different types of therapies, including cytotoxic chemotherapy and cell-based immunotherapies, which impact the size of the tumor cell or immune cell populations, and immune checkpoint inhibitors, which impact the nature of the interactions between tumor and immune cell populations. They also addressed potential outcomes to combination therapies.
These models help conceptualize how therapies can be combined to achieve optimal outcomes for patients through immune-cell control of tumor cell populations. In the future, the researchers hope mathematical modeling can be used in the clinic to help predict patient responses to therapy and guide treatment.
"Mathematical oncology abstraction provides a novel and promising way to conceptualize the effect of various cancer treatments on a patient's tumor and the local immune environment and gives us an opportunity to rethink the immunotherapy numbers game," said Heiko Enderling, Ph.D., study author and associate member of the Integrated Mathematical Oncology Department at Moffitt.
More information: Rebecca A Bekker et al, Rethinking the immunotherapy numbers game, Journal for ImmunoTherapy of Cancer (2022). DOI: 10.1136/jitc-2022-005107


















