Insufficient insulin processing leads to obesity
Obesity increases the risk of an imbalance in sugar metabolism and even of diabetes. A research group at the University of Basel has now shown the opposite is true as well: deficits in the body's insulin production contribute to obesity.
Poor nutrition, too little movement and too many pounds on the scale—lifestyle influences the risk of metabolic diseases like diabetes. But the relationship works the other way around as well, as a research group led by Dr. Daniel Zeman-Meier of the university's Department of Biomedicine and the University Hospital of Basel reports. If insulin production is compromised, as is the case in the early stages of type 2 diabetes, this can contribute to obesity. The researchers report their findings in the journal Nature Communications.
The research team focused on protease PC1/3, a key enzyme in the body that transforms various inactive hormone precursors into the final, active forms. If this enzyme isn't functioning properly in a person, the result can be severe endocrine disorders. The consequences include a feeling of uncontrollable hunger and severe obesity.
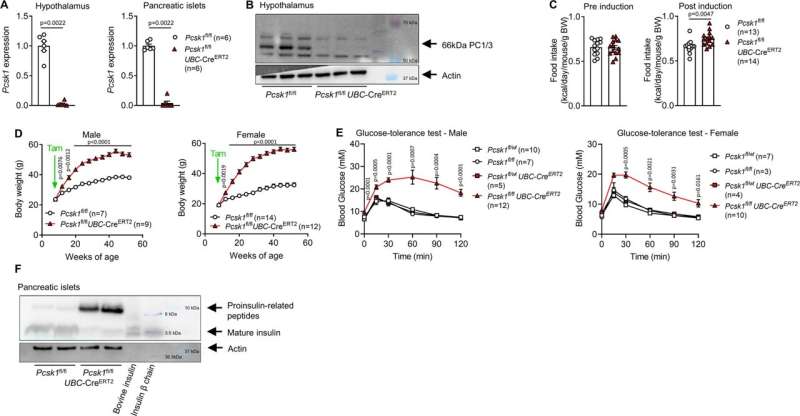
"Until now, it was assumed that this dysregulation is caused by a lack of activation of satiety hormones," explains the study's leader, Dr. Zeman-Meier. "But when we turned off PC1/3 in the brains of mice, the animals' body weight did not change significantly." The researchers concluded from this that something other than a brain malfunction must be responsible.
Incorrect activation of insulin leads to hunger and obesity
In their next step, they tested whether obesity could be caused by incorrect activation of other hormones. PC1/3 activates insulin, among other things. Insulin plays a key role in the regulation of blood sugar and fat metabolism. "Investigating the role of insulin production as a cause of obesity was obvious," says Dr. Zeman-Meier.
The researchers shut off PC1/3 specifically in the insulin-producing beta cells of the pancreas in mice. The animals consumed significantly more calories and soon became obese and diabetic.
"These results are also interesting because PC1/3 is reduced in the pancreas of patients with prediabetes," says Professor Marc Donath, the research group leader and final author of the study. This indicates that incorrect insulin activation could be not only a consequence, but also a cause of obesity.
But PC1/3 is also important in the weight regulation of healthy individuals, Donath says. The researchers were able to show that the gene expression of PC1/3 in the pancreas is negatively correlated with body weight in the general population—meaning that sufficient PC1/3 promotes a healthy body weight.
The finding that a defect in the insulin-producing beta cells is a trigger of obesity opens up new therapeutic possibilities. For example, it is conceivable that medications could be used to reduce the production of immature insulin precursors, creating a new tool in the fight against obesity and diabetes.
More information: Daniel T. Meier et al, Prohormone convertase 1/3 deficiency causes obesity due to impaired proinsulin processing, Nature Communications (2022). DOI: 10.1038/s41467-022-32509-4





















