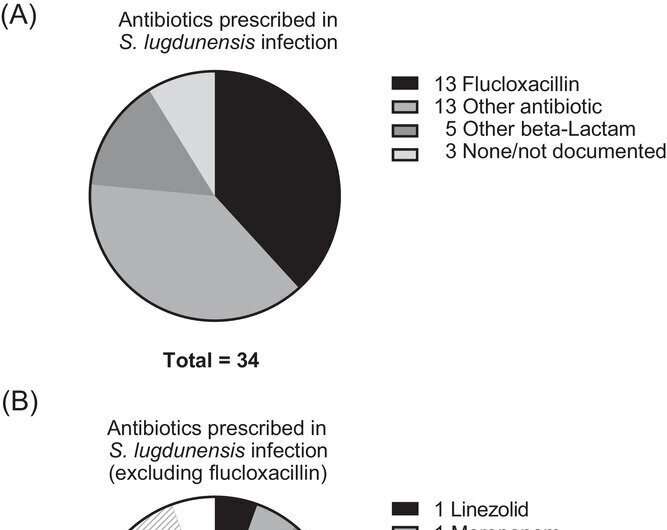
(A) Summary of antibiotics prescribed for S. lugdunensis infection. (B) Non-flucloxacillin antibiotics prescribed. Credit: Pediatric Investigation (2022). DOI: 10.1002/ped4.12345
Staphylococcus lugdunensis is a coagulase-negative staphylococci (CoNS), commonly found on human skin. While most CoNS bacteria are typically considered clinically harmless, recent studies have shown S. lugdunensis can be as virulent as S. aureus—another important disease-causing bacterium.
Like S. aureus, S. lugdunensis is associated with skin and soft tissue infections and is being increasingly seen as a major cause of periprosthetic joint infections, especially when metals are used for making prosthetic devices. These infections usually require prolonged antimicrobial treatment to overcome the source infection.
The occurrence of S. lugdunensis in the pediatric population was considered to be uncommon, and there were very few studies on S. lugdunensis infections in children, until now. In a recent study published in Pediatric Investigation, researchers from the UK, led by Dr. Thomas Patrick Bowman from the Department of Cardiology, University Hospital Ayr, have analyzed the local rates, risk factors, and demographics of S. lugdunensis infection in children.
As Dr. Bowman explains, "Most clinical guidelines for the management of S. lugdunensis infection are based on data concerning adult patients. So, we specifically dove deeper into infection rates and sensitivity patterns in the pediatric population."
For their analysis, the researchers sourced data on S. Lugdunensis isolates for the period between 2015 and 2020 from the tertiary pediatric center at NHS Glasgow and Clyde. These isolates had all been identified using Matrix-Assisted Laser Desorption Ionization and Time Of Flight Mass Spectroscopy (MALDI-TOF-MS).
"2015 was when the local microbiology lab first used MALDI-TOF-MS technology. Compared to previous biochemical methods, MALDI-TOF-MS has greatly increased the accuracy of identification of CoNS bacteria," says Dr. Bowman. S. lugdunensis displays high colonization–it grows rapidly on the host without any clinical expression or symptoms—and this was why it was necessary to accurately identify the samples for clinical infection, not colonization, explained Dr. Bowman.
The researchers found that a large number (around 68%) of the S. lugdunensis isolates were sourced from a skin infection. Interestingly, although their numbers were small, there were infections whose source could be traced to the central nervous system (CNS). Describing the connection between S. lugdunensis infections and the CNS, Dr. Bowman explains, "CNS infections appear to be a significant source of S. lugdunensis—in our analysis, all three isolates cultured from cerebrospinal fluid were from cases managed as infections."
Importantly, each of these three cases was linked to infection in a ventriculoperitoneal (VP) shunt—a surgically inserted cerebral shunt used to treat hydrocephalus by draining excess cerebrospinal fluid. The team did not identify any cases of endocarditis with infective S. lugdunensis, and flucloxacillin resistance was identified in about 19% of S. lugdunensis isolates.
The finding that individuals carrying S. lugdunensis did not present a clear infection supports the known high rate of S. lugdunensis colonization in patients. The data revealed that 47 out of 86 NICU patients who were less than a year old, were colonized by S. lugdunensis in the first 7 days but did not display neonatal complications.
On the contrary, nearly 67% of the patients with complications from birth contained S. lugdunensis isolates after the first 7 days, suggesting colonization were driven by prolonged and intensive medical management.
Their results confirm that flucloxacillin can be used locally and is suitable as a first-line antimicrobial in non-critical situations. So where does the team go from here? The researchers believe they have laid the foundation for work that aims to understand the mechanisms underpinning S. lugdunensis resistance, and the role of the bacterium in CNS infections.
"We've been able to identify some of the possible risk factors like age, significant musculoskeletal medical history, and VP shunt placement that are driving infections in pediatric settings," concludes Dr. Bowman.
More information: Thomas Patrick Bowman et al, Staphylococcus lugdunensis in children: A retrospective analysis, Pediatric Investigation (2022). DOI: 10.1002/ped4.12345
Provided by Cactus Communications