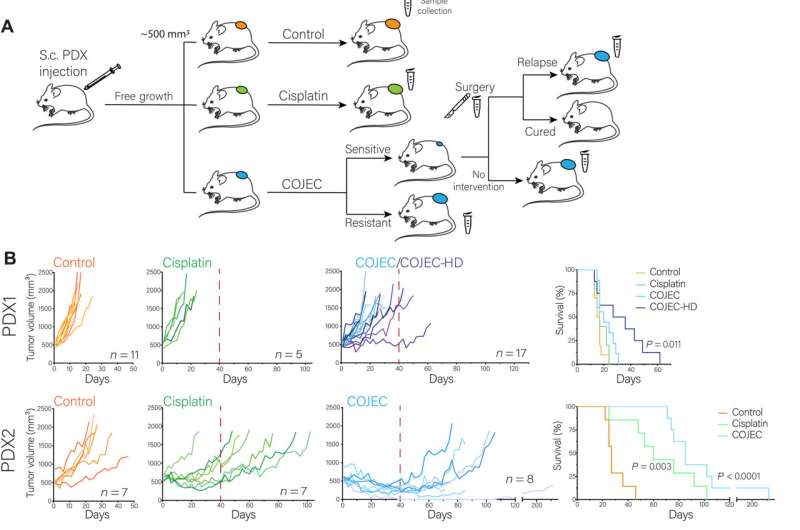
Establishment and application of a COJEC-like treatment protocol using NB PDX models.(A) Schematic representation of the experimental design. Mice were injected subcutaneously (S.c.) with dissociated PDX-derived organoids from PDX 1, 2, or 3. When tumors reached ~500 mm3, mice were randomized into groups: control, cisplatin, and COJEC. A subgroup of PDX3 COJEC–responsive mice was further subjected to tumor resection surgery. Scalpel symbol represents the surgery branch. Microtube symbol represents sample collection time points. (B) Tumor volume and mouse survival for each PDX model for the different treatment protocols. Red dashed line represents the end of treatment. HD, high-dose group for PDX1. Statistical analysis of survival was performed with log-rank test. (C) Immunohistochemical staining of PHOX2B (NB marker). (D) Representative hemotoxylin and eosin (H&E) and TUNEL staining for PDX3. (E) Assessment of differentiation status based on morphology from H&E staining. (F) Quantitation of cell death from TUNEL assay. (G and H) Quantitation of morphological differentiation and Ki67-positive cells for samples that were or were not cured in PDX3 in the surgery group. Scale bars, 50 μm. Credit: Science Advances (2022). DOI: 10.1126/sciadv.abq4617
Researchers at Lund University in Sweden have identified one of the reasons why the childhood cancer neuroblastoma becomes resistant to chemotherapy. The findings are significant for how future treatments should be designed. The results have been published in Science Advances.
Neuroblastoma is an aggressive cancer of the sympathetic nervous system, especially of the adrenal gland. Despite intense treatment with chemotherapy, the disease can be difficult to cure and the prognosis is poor for children who have the aggressive variant. One of the reasons is that the tumor often develops resistance to drugs. In order to understand what happens when the tumor becomes resistant, good disease models are needed that can mimic the complex drug treatment given to patients today:
"Tumors from patients with neuroblastoma look very different, and it is difficult to produce a model that is representative of many patients. This type of challenge often limits medical research," explains the study's first author, Adriana Mañas, child cancer researcher at Lund University.
However, the researchers have now succeeded in developing a model in mice with human neuroblastoma tumor cells, which makes it possible to follow the mechanisms that occur when certain tumor cells develop resistance to drugs.
"What happens is that the tumor cells change to mimic embryonic cells from the fetal development phase. These embryonic tumor cells are more resistant to chemotherapy," says research group leader Daniel Bexell, who led the study.
It has long been known that genetic changes are crucial for neuroblastoma to form and develop into an aggressive tumor. However, when it comes to resistance, it is not primarily about genetic changes, but rather that the cells quickly adapt their behavior. The reason why the embryonic tumor cells are less responsive to drugs is not yet fully understood, but the researchers think that that the cells in their immature state can adapt and survive in changing conditions.
"Current treatment with chemotherapy targets rapidly dividing tumor cells. Our research results can contribute to new treatments which better reach the entire tumor, in order to avoid the development of resistance. In future research, it will be important to understand how to specifically target the embryonic state of the neuroblastoma cell in order to cure patients," concludes Daniel Bexell.
More information: Adriana Mañas et al, Clinically relevant treatment of PDX models reveals patterns of neuroblastoma chemoresistance, Science Advances (2022). DOI: 10.1126/sciadv.abq4617
Journal information: Science Advances
Provided by Lund University