Graphical abstract. Credit: Clinical Immunology (2022). DOI: 10.1016/j.clim.2022.109209
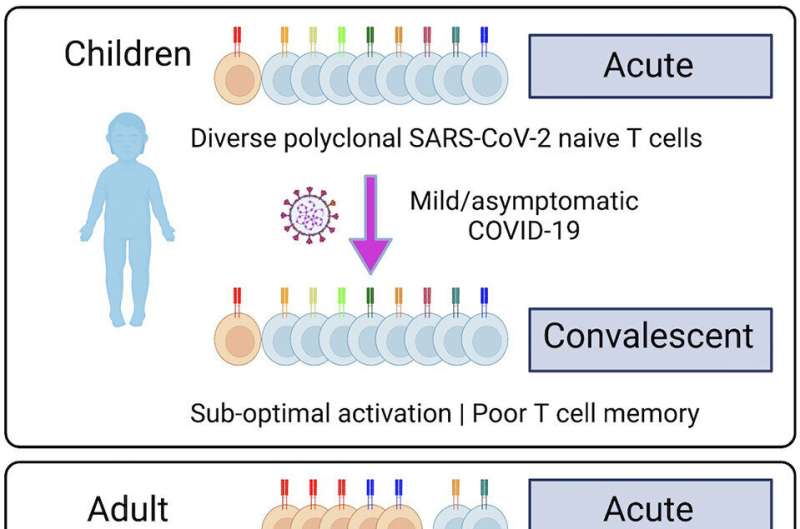
Children have largely avoided severe COVID-19 symptoms because they have a strong initial 'innate' immune reaction that quickly defeats the virus. And now, researchers led by scientists at the Garvan Institute of Medical Research have uncovered what this might mean for the immune system. Unlike those of adults, children's immune systems don't remember the virus and don't adapt, so when they're next exposed to SARS-CoV-2, their body still treats it as a new threat, the scientists found.
"The price that children pay for being so good at getting rid of the virus in the first place is that they don't have the opportunity to develop 'adaptive' memory to protect them the second time they are exposed to the virus," says lead author Professor Tri Phan, Head of the Intravital Microscopy and Gene Expression (IMAGE) Lab and Co-Lead of the Precision Immunology Program at Garvan.
"Because children haven't been exposed to many viruses, their immune system is still 'naïve.' And because they don't develop memory T cells, they are at risk of getting sick when they become reinfected. With each new infectious episode as they get older, there is a risk of their T cells becoming 'exhausted' and ineffective, like the T cells in older people. This is why we think it's important to vaccinate children," he says.
The immune system has two modes. The innate immune system is the first line of defense, comprising physical barriers such as skin and mucosal surfaces that block viruses from entering. It is also composed of cells that make chemicals to signal to other cells and ward off the viruses. The innate immune system does not distinguish between one type of virus or another.
The second line of defense comprises B and T cells of the adaptive immune system. These cells have specific receptors that can recognize and distinguish different parts of a virus and generate a rapid response to neutralize or limit it.
Infants start with an immune system blank slate, which has a much higher proportion of naïve T cells, the researchers found. As they move through childhood into adulthood and become exposed to more viruses, the naïve T cells are replaced by memory T cells that are locked in to making responses to viruses they have seen before.
"Over time, as you get infections, your immune system becomes more 'educated,' allowing you to make a faster immune response that's tightly matched to the viruses that have infected you before," says Associate Professor Philip Britton, pediatric infectious diseases physician at the Children's Hospital at Westmead, and clinical lead in the study. "Children's immune systems move from relying mostly on the innate system, to needing the adaptive system as a backup as they grow older and are unable to clear viruses as rapidly."
In the new study, published in the journal Clinical Immunology, Professor Phan, Associate Professor Britton and colleagues took a deep dive to investigate T cells and cellular immune responses of a small group of children and their household family contacts who had mild or no symptoms from coronavirus (SARS-CoV-2) infection.
The researchers sequenced white blood cell samples to analyze T cells in children and adults at the time of acute infection and one month later.
Because they studied household family contacts who were infected, researchers could control for the impact of genetic or environmental influences on the immune response.
They found that children had many different naïve T cells to fight SARS-CoV-2 and made poor memory T cell responses to the virus after they had recovered, whereas the adults had few naïve T cells but made good memory T cell responses after recovery.
Interestingly, the findings point to why older adults can have a kind of immune over-reaction to SARS-CoV-2.
"When adults are infected for the first time with SARS-CoV-2, their memory T cells recognize only what they've seen before—like a familiar part of the coronavirus that is shared with the common cold coronaviruses," Professor Phan says.
"This may lock the immune system in to a misdirected response that is not specific to SARS-CoV-2. It provides an opportunity for the virus to escape and multiply unchecked to cause more severe symptoms as the immune system ramps up to try and fix the problem."
More information: Weng Hua Khoo et al, Tracking the clonal dynamics of SARS-CoV-2-specific T cells in children and adults with mild/asymptomatic COVID-19, Clinical Immunology (2022). DOI: 10.1016/j.clim.2022.109209
Journal information: Clinical Immunology
Provided by Garvan Institute of Medical Research