This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
New definitions of multimorbidity may improve clinical decision-making for older surgical patients
A new way to identify more specific, higher-risk groups of older surgical patients can help in clinical decision-making and accurately comparing the performance of one hospital to another, according to research published in the Journal of the American College of Surgeons.
Multimorbidity in surgical patients is defined as multiple comorbidities or chronic conditions that are common and associated with worse postoperative outcomes. Conventional multimorbidity definitions offer limited clinical usefulness because they label the vast majority of older patients as "multimorbid," do not specify which comorbidities are contributing to the risk, and do not incorporate the patient's functional status.
The new study developed and validated better surgical, specialty-specific, multimorbidity definitions based on distinct comorbidity combinations for older inpatient general, orthopedic, and vascular surgery patients. The new definitions were able to specify high-risk comorbidity combinations that contribute to patient risk while also addressing patients' functional status, said the study's lead author Omar I. Ramadan, MD, MSc, a general surgery resident at the University of Pennsylvania Perelman School of Medicine in Philadelphia.
"Ultimately, our multimorbidity methodology is a powerful way to assess risk and it's easy to apply because it uses administrative datasets," Dr. Ramadan said.
Multimorbidity definitions
Using Medicare administrative claims data, the researchers analyzed patients aged 66-90 years undergoing either inpatient general, orthopedic, or vascular surgery procedures between 2016 and 2017 to develop the multimorbidity definitions. The researchers then analyzed patients between 2018 and 2019 to validate the definitions.
These patients were categorized into clinically relevant groups by ICD-10 principal procedure codes. In the development of the definitions for multimorbidity, the researchers did not include patients with metastatic cancer, Alzheimer's disease and related dementias, or who were 90 years or older.
These conditions are already associated with high mortality rates and patients with them would possibly have different goals of care if faced with severe postoperative complications. However, patients with these characteristics were studied using their new multimorbidity definitions.
The researchers defined multimorbidity as the presence of one or more qualifying comorbidity sets (QCSs). QCSs, in turn, were defined as combinations of one to three comorbidities that were associated with at least 2-fold (for general and orthopedic surgery patients) or 1.5-fold (for vascular surgery patients) greater risk of 30-day mortality compared to patients in the same age group undergoing the same procedure.
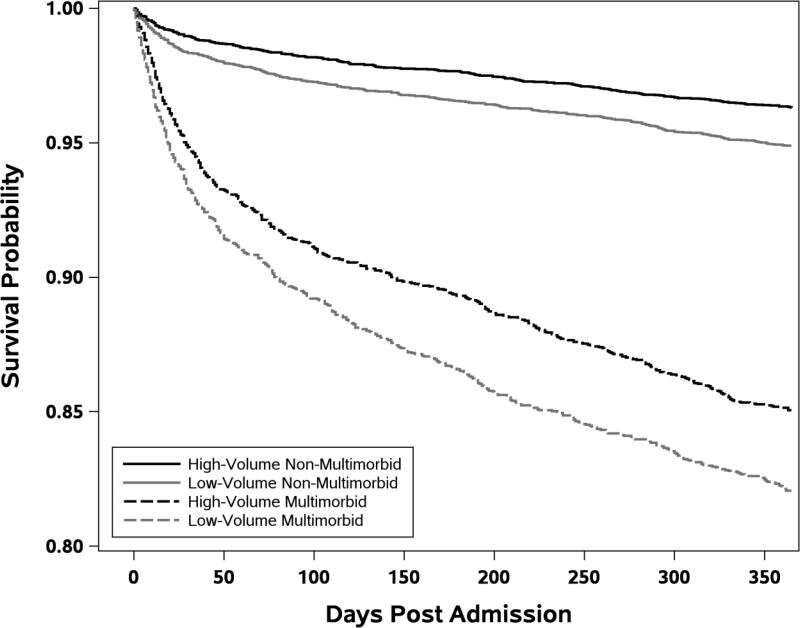
For further validation, the researchers tested whether patients with multimorbidity had different outcomes based on hospital quality since it is well established that higher-quality hospitals are associated with better outcomes for high-risk patients. The researchers defined higher-quality hospitals as those with a nursing skill mix and surgical, specialty-specific patient volume above the median as well as resident-to-bed ratios (>0.25) characteristic of major or very major teaching hospitals.
Key study findings
Compared to conventional multimorbidity definitions, the new definitions labeled far fewer patients as multimorbid: for general surgery, the new definition identified 55.9% of the older population compared to 85.0% (conventional); for orthopedic surgery, 40.2% (new) versus 55.9% (conventional); and for vascular, 52.7% (new) versus 96.2% (conventional).
Thirty-day mortality was higher in the new definitions: general surgery, 5.64% (new) versus 3.96% (conventional); orthopedic surgery, 1.68% (new) versus 1.13% (conventional); and vascular, 7.00% (new) versus 4.43% (conventional). The researchers also found that higher-quality hospitals offered significantly greater mortality benefits than other hospitals for multimorbid versus non-multimorbid general and orthopedic, but not vascular, patients, in keeping with prior literature.
The study showed that the highest risk (30-day mortality) QCS for general surgery was home hospital bed or wheelchair use combined with thrombocytopenia and other hematological disorders; for orthopedic surgery, protein-calorie malnutrition; and for vascular surgery, acute heart or respiratory failure.
"I was surprised at how profound the increases in mortality were for some of these QCSs," Dr. Ramadan said. "For example, in general surgery, a patient who is wheelchair or hospital bed bound and has thrombocytopenia and other hematological disorders is 18 times more likely to die within 30 days than a patient who is not multimorbid undergoing the same procedure."
New definition could help patients, surgeons, and policymakers
The new multimorbidity definitions will help surgeons better explain the risks associated with any given procedure to patients and to make better care decisions, Dr. Ramadan said. For policymakers and hospital systems, the definitions offer a better way of benchmarking and accurately comparing the performance of one hospital to another, he also said.
Research using the new multimorbidity definitions is continuing in several areas, including how to use the definitions to compare hospital systems with each other, and how to use them to quickly assess a patient's risk for any given surgical procedure, Dr. Ramadan said.
More information: Omar I Ramadan et al, Redefining Multimorbidity in Older Surgical Patients, Journal of the American College of Surgeons (2023). DOI: 10.1097/XCS.0000000000000659





















