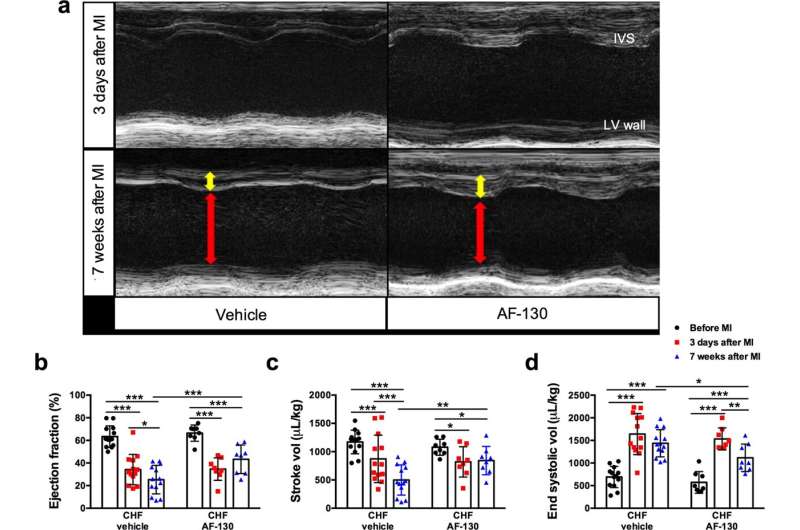
P2X3-receptor antagonism improves cardiac function in chronic heart failure (CHF) rats. a Representative images of echocardiography in rats submitted to myocardial infarction (MI), before and after 7 weeks of treatment with vehicle or AF-130. Red arrows indicate diastolic ventricular diameter and yellow arrows indicate diastolic ventricular wall thickness. P2X3-receptor antagonism prevented the reduction of ejection fraction (b) and stroke volume (c) during HF development, and reduced left ventricular (LV) end-systolic volume (d). The parameters were analyzed before MI surgery, three days after MI and after 7 weeks of vehicle (n = 13) or AF-130 (n = 8) administration. IVS: interventricular septum. Data are mean ± SD. Repeated measures two-way ANOVA, with Student-Newman-Keuls post hoc comparison. *P < 0.05, **P < 0.01, ***P < 0.001. Credit: Nature Communications (2023). DOI: 10.1038/s41467-023-37077-9
A novel drug is showing promise for alleviating heart failure, a common condition associated with sleep apnea and a reduced lifespan. The drug, known as AF-130, was tested in an animal model at Waipapa Taumata Rau, the University of Auckland where researchers found it improved the heart's ability to pump, but, equally important, prevented sleep apnea, which itself reduces lifespan. The work is published in the journal Nature Communications.
"This drug does offer benefit for heart failure, but it's two for the price of one, in that it's also relieving the apnea for which there is currently no drug, only CPAP (a breathing device), which is poorly tolerated," says Professor Julian Paton, director of the University's Manaaki Manawa, Center for Heart Research.
When a person has a heart attack and subsequent heart failure, the brain responds by activating the sympathetic system, the "fight or flight" response, as a way to stimulate the heart to pump blood. However, the brain persists with this activation of the nervous system, even when it is no longer required, and this together with the consequent sleep apnea, contributes to the patient's reduced life expectancy. Most patients die within five years of a heart failure diagnosis.
"This study has revealed the first drug to temper the nervous activity from the brain to the heart thereby reversing the heart's progressive decline in heart failure," says Professor Paton.
The part of the brain that sends nervous impulses to the heart is also controlling respiration, so this drug has a dual function, reducing the "fight or flight" response while also stimulating breathing to stop the sleep apnea. "These findings have real potential for improving the wellness and life expectancy of almost 200,000 people living with heart disease in Aotearoa New Zealand," says Professor Paton.
Another exciting factor for the scientists, who are from the University of Auckland and the University of São Paulo, Brazil, is that the drug is soon to be FDA approved, albeit for a different health issue, paving the way for human trials in the next year or two, Professor Paton says.
"Over recent decades there have been several classes of drugs that have improved the prognosis of heart failure," says cardiology consultant and Associate Professor, Martin Stiles. "However, none of these drugs work in the way that this new agent does. So it is exciting to see a novel method that potentially reverses some features of heart failure."
More information: Renata M. Lataro et al, P2X3 receptor antagonism attenuates the progression of heart failure, Nature Communications (2023). DOI: 10.1038/s41467-023-37077-9
Journal information: Nature Communications
Provided by University of Auckland