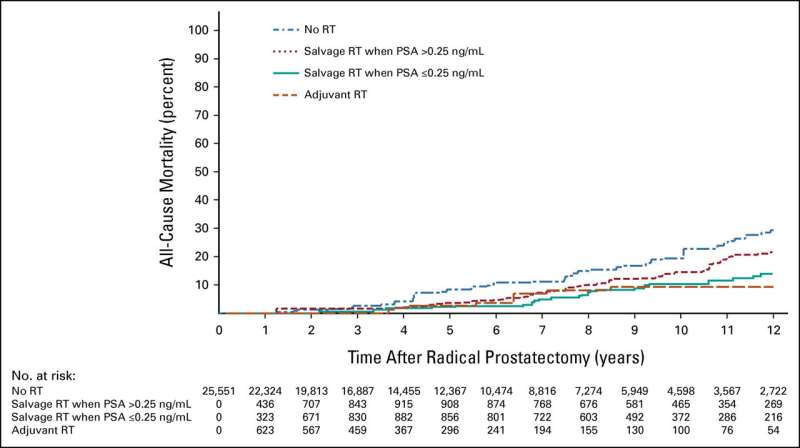
Adjusted estimates of ACM among men illustrating the difference in these estimated among patients in the time-dependent treatment groups of no RT, aRT, salvage RT when the PSA level >0.25 ng/mL compared with salvage RT when the PSA level is ≤0.25 ng/mL after RP (baseline). ACM, all-cause mortality; aRT, adjuvant RT; ng/mL, nanograms/milliliter; PSA, prostate-specific antigen; RP, radical prostatectomy; RT, radiation therapy. Credit: Journal of Clinical Oncology (2023). DOI: 10.1200/JCO.22.02489
The performance characteristics of prostate-specific membrane antigen positron emission tomography improves with increasing prostate-specific antigen (PSA) level. This, coupled with insurance approval concerns if applied for too early, causes some physicians to delay post-radical prostatectomy salvage radiation therapy (sRT) until well after PSA failure, typically at PSA levels exceeding 0.30 ng/ml.
To determine whether such a delay increases mortality risk, a multinational group led by researchers from Dana-Farber Brigham Cancer Center studied radical prostatectomy and lymph node specimens from 25,551 patients with no more than one high-risk factor (prostatectomy Gleason score of 8–10 or evidence at surgery of extension of the cancer outside the prostate). They sought to identify a PSA level above which initiating sRT is associated with increased mortality risk.
The research team used multivariable Cox regression analysis beginning at a PSA level of 0.10 ng/mL and in 0.05 increments up to 0.50 ng/mL versus at or below that level. The model was adjusted for age at and year of surgery, established prostate cancer prognostic factors, institution, and time-dependent use of androgen deprivation therapy.
The study found that after a median follow-up of six years, patients who received sRT at a PSA level higher than 0.25 ng/mL had approximately a 50 percent higher risk of death compared with those who received sRT when the PSA was at or below 0.25 ng/ML.
"At Dana-Farber Brigham, we tend to be more medically conservative and not allow these restraints to drive patients to a lower cure rate," said principal investigator Anthony Victor D'Amico, MD, Ph.D., chief of Genitourinary Radiation Oncology, Dana-Farber Brigham Cancer Center. "Normally, we would want to start sRT at a PSA level of 0.2, or even 0.1 ng/ml in most cases, to decrease the risk of the cancer metastasizing or becoming resistant to existing salvage treatments such as radiation and androgen deprivation therapy and to maximize curability."
The paper is published in the Journal of Clinical Oncology.
More information: Derya Tilki et al, Prostate-Specific Antigen Level at the Time of Salvage Therapy After Radical Prostatectomy for Prostate Cancer and the Risk of Death, Journal of Clinical Oncology (2023). DOI: 10.1200/JCO.22.02489
Journal information: Journal of Clinical Oncology
Provided by Brigham and Women's Hospital