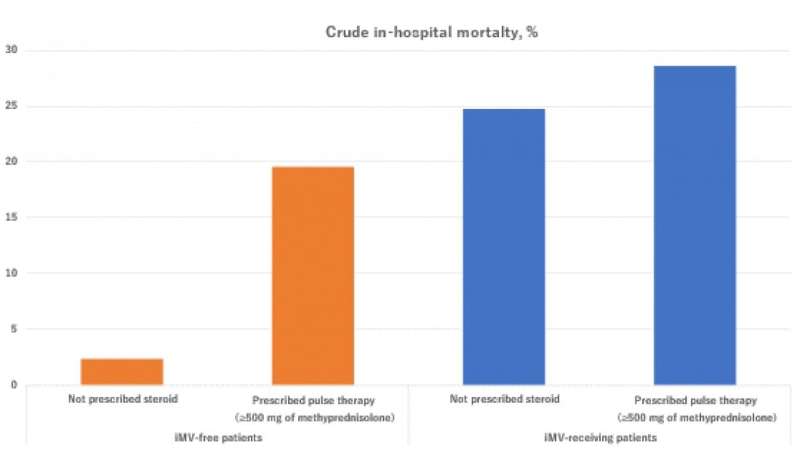
Fig. 1. Without bias control: Univariate in-hospital mortality in patients prescribed or not prescribed methylprednisolone pulse therapy, stratified by the presence or absence of invasive mechanical ventilation (iMV). Credit: R.Sakaniwa and T.Moromizato at el.,
Although steroid treatment for COVID-19 is reportedly beneficial in some cases, details—such as the upper dosing limits and safety of this method—have not yet been clarified. Now, Japanese researchers have used a large dataset and complicated statistical methods to iron out the specifics of this treatment.
In a study published last month in Critical Care, researchers from Osaka University revealed that when repeated high doses (known as pulse therapy) of steroid methylprednisolone were given to patients receiving invasive mechanical ventilation, the patients were more likely to die; however, the opposite was true when the researchers corrected the data for underlying bias.
Steroid pulse therapy can reduce inflammation in many diseases and improve patient outcomes but can also cause fatal complications. Previous studies have reported different and sometimes conflicting results with pulse steroid therapy, which may be because many patients receive the treatment as a kind of "Hail Mary" —meaning the situation is so grave that doctors and family members are willing to try anything to save the patient. This can distort the associations between treatment and outcome, something that the researchers from Osaka University wanted to tackle head-on.
"We were lucky that we had access to data from 67,348 hospitalized COVID-19 patients across 438 hospitals in Japan," says Professor Yasuharu Tokuda, corresponding author of the study. "This large dataset allowed us to use a relatively new statistical model, known as marginal structural model analysis, to look at the outcomes of pulse therapy in different kinds of COVID-19 patients in an unbiased manner."
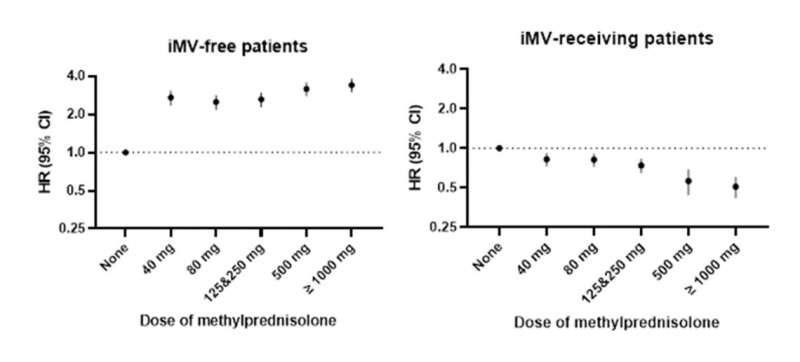
Fig. 2. With bias control: Forest plots of hazard ratios (HRs) and 95% confidence intervals (95% CIs) for the risk of in-hospital mortality among acute COVID-19 patients with or without invasive mechanical ventilation (iMV) after doses of 40, 80, 125–250, 500, and 1000 mg and more of intravenous methylprednisolone. Credit: R.Sakaniwa and T.Moromizato at el., Critical Care 2023, CC BY
When the data were analyzed without the bias control, the researchers found that methylprednisolone pulse therapy was clearly associated with increased in-hospital mortality in patients receiving invasive mechanical ventilation, from 24.7% to 28.6%. In patients who didn't receive invasive mechanical ventilation, pulse therapy also increased the in-hospital mortality rates, from 2.3% to 19.5% (Fig. 1). However, when the research team had taken into account the "Hail Mary bias" (there is also named time-dependent bias) at the data using the cutting-edge analysis, steroid pulse therapy was associated with a lower risk of mortality among COVID-19 patients receiving invasive mechanical ventilation but an increased risk among patients not receiving ventilation (Fig. 2).
"Optimal assessment methods are important when analyzing the results of COVID-19 studies. Here, we found that appropriate patient selection is key when considering methylprednisolone pulse therapy for hospitalized patients," explains primary co-author, Dr. Ryoto Sakaniwa. "We also found that higher doses of methylprednisolone and a relatively short interval between patient intubation and the start of pulse therapy were associated with better outcomes in patients receiving ventilation, which will further improve COVID-19 treatments."
Measures must be taken to stop COVID-19 from taking more lives. This study adds valuable new information on the treatment of COVID-19, which can be potentially applied globally to reduce in-hospital mortality associated with COVID-19. Better knowledge of the optimal conditions for pulse methylprednisolone therapy will improve outcomes for all future COVID-19 patients.
More information: Takuhiro Moromizato et al, Intravenous methylprednisolone pulse therapy and the risk of in-hospital mortality among acute COVID-19 patients: Nationwide clinical cohort study, Critical Care (2023). DOI: 10.1186/s13054-023-04337-5
Journal information: Critical Care
Provided by Osaka University