This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
States with high COVID-19 death rates also saw high mortality from other causes
During the first year of the pandemic, states in the U.S. with high rates of death from COVID-19 saw significant increases in other causes of death, too, including cardiovascular disease, dementia, diabetes, and influenza. That's according to findings from the University of Pennsylvania, Boston University, and the Robert Wood Johnson Foundation published recently in the journal PLOS ONE.
"States with a high burden of mortality from COVID suffered from a higher burden of mortality all around," says Penn demographer Samuel Preston, senior paper author. "We anticipated that this relationship might show up."
The work sheds light on one of the pandemic puzzles for demographers. Since the COVID-19 virus emerged, non-COVID deaths have accounted for a significant amount of total excess mortality, or the number of people who died for any reason above and beyond what would have been expected under normal circumstances. "We decided we needed to capture a fuller picture of how the pandemic contoured the mortality landscape in the United States," says Anneliese Luck, a Penn doctoral student and first author on the paper. "We wanted to look beyond COVID-19 deaths."
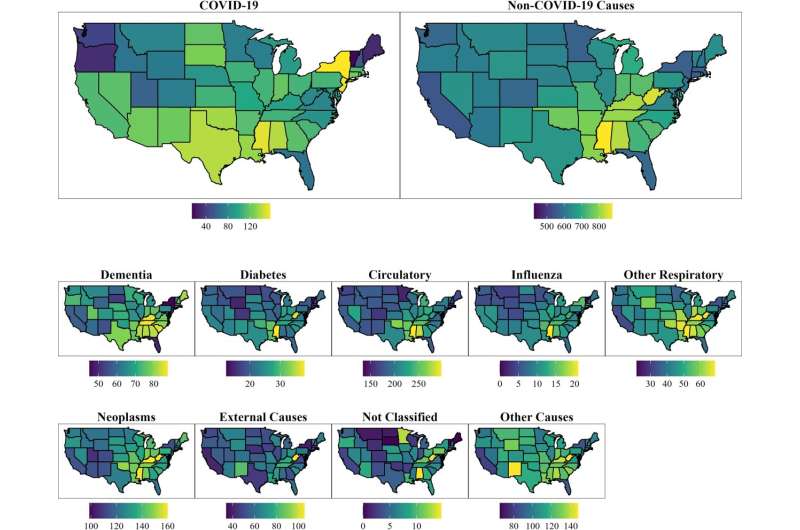
To find cause-specific mortality data, Luck and colleagues turned to a database from the Centers for Disease Control and Prevention called WONDER, which stands for Wide-ranging ONline Data for Epidemiologic Research. They also pulled population statistics from the U.S. Census Bureau. Then, for the period between March 2020 and February 2021, for all states and Washington, D.C., the researchers calculated death rates for three age groups and nine underlying causes.
Their analysis showed that non-COVID causes explain about 20% of excess mortality during that time frame. More specifically, for those 25 and older, circulatory disease accounted for more than 50% of this, with dementia, influenza/pneumonia, and diabetes also playing a role. "The real anomaly is cancer," Preston says. "States with unusually high death rates from COVID had unusually high declines in death rates from cancer. I don't think most people would have anticipated that."
Though the data don't explain the reason for these findings, Preston, Luck, and co-author Andrew Stokes, an assistant professor at BU, offer several possible explanations. For one, states with high COVID death rates likely had unusually crowded medical facilities pressed in their ability to handle routine medical issues. Plus, fear over what was then a new and scary virus called COVID-19 may have prevented people from seeking care.
Second, the researchers say deaths may have been miscoded on death certificates. "This is particularly likely when there is a synergistic relationship between a disease process and COVID, like someone with preexisting cardiovascular disease being more susceptible to the virus," Preston says. "When that person dies, the death may be as likely assigned to the preexisting heart disease as it is to COVID." Beyond that, their data also revealed that certain parts of the country underreported COVID deaths.
"Our study clearly shows that mortality associated with the COVID epidemic is underestimated," Preston says.
"That's the bottom line," says Stokes, who notes that such misclassification often keeps communities in the dark. "Gaps in reporting or deaths not being registered as COVID deaths could mean communities aren't fully aware of the severity of the pandemic there," he says. "The pandemic is at least partially hidden from view."
Though the researchers haven't studied whether this trend continued beyond the pandemic's first year, they say that the findings indicate a need for better cause-of-death coding. And, given that states serve as key drivers in shaping the policies that affect how people live and seek medical care, the researchers also suggest a more focused exploration of state-level differences in health care utilization, in particular looking at sociodemographic, behavioral, and environmental characteristics across the U.S. "We hope our findings call attention to the pandemic's full mortality burden," Luck says, "and help inform how states continue responding to the ongoing COVID-19 crisis."
More information: Anneliese N. Luck et al, Associations between mortality from COVID-19 and other causes: A state-level analysis, PLOS ONE (2023). DOI: 10.1371/journal.pone.0281683




















