This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Survey of family physicians identifies gaps in primary care's behavioral health integration
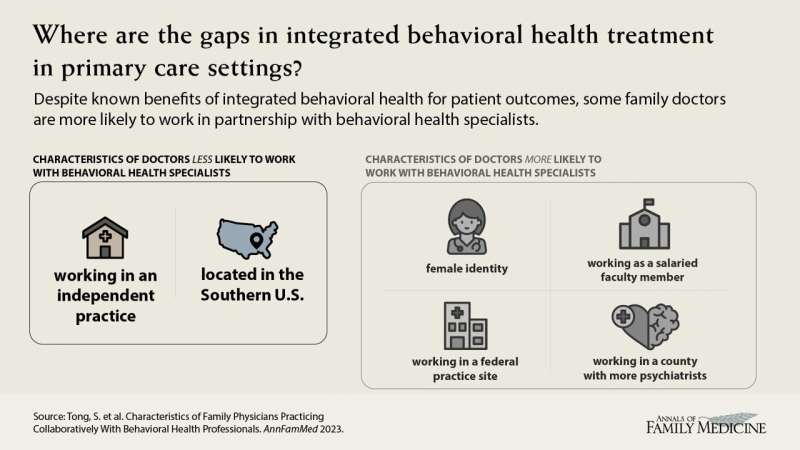
In an article published in The Annals of Family Medicine, researchers from the American Board of Family Medicine (ABFM) and the University of Washington in Seattle examined the characteristics of family physicians who work collaboratively with behavioral health professionals (BHP). Prior evidence has demonstrated that integrating behavioral health into primary care can improve access to mental health care and patient health outcomes.
Almost 40% (38.8%) of 25,222 family practitioners reported working collaboratively with behavioral health professionals. Physician characteristics significantly associated with increased odds of BHP collaboration were being female (OR 1.09) and working as core/salaried faculty (OR 2.32) as compared to non-faculty. The strongest practice characteristic was working in a federally run practice site and the strongest negative association was working in an independently owned practice and being located in the Southern United States. Additionally, working in a county with more psychiatrists is associated with higher likelihood of BHP collaboration. Understanding these disparities could help improve behavioral health access for patients and improve overall patient outcomes.
Integrated behavioral health has been shown to improve mental health and overall health outcomes, patient care experience and clinician satisfaction, while reducing health care use and costs. However, not all family medicine practices offer integrated behavioral health services.
Almost 40% of family practitioners work collaboratively with behavioral health professionals. Physicians who were female; worked as core/salaried faculty; and worked in a federal practice site were more likely to work with integrated behavioral health. Gaps in access to integrated behavioral health were seen in independently owned practices and those located in the Southern United States.
More information: Sebastian T. Tong et al, Characteristics of Family Physicians Practicing Collaboratively With Behavioral Health Professionals, The Annals of Family Medicine (2023). DOI: 10.1370/afm.2947


















