April 10, 2023 report
This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Gut microbiota, Alzheimer's and the central nervous system
University of Nevada, Las Vegas, researchers have identified a correlation between Alzheimer's disease and specific gut microbiota populations. In a paper published in Scientific Reports titled "Genetic correlations between Alzheimer's disease and gut microbiome genera," the researchers explain how they narrowed the search down to a half dozen disease-correlated microbes, with one related to the most significant risk.
The study authors point to a growing body of research suggesting that disruptions in regular ratios and lower diversity of gut microbiota are associated with neurodegenerative diseases via neuroinflammatory processes across the microbiota-gut-brain axis. Previous studies have also indicated that Alzheimer's patients have just such reduced microbiome diversity.
Researchers used polygenic risk scores, a risk assessment based on known genetic correlations to disease, of 119 microbiome species for each individual from a discovery sample of 1,278 cases with 1,293 controls. They found that 20 out of the 119 genera were significantly associated with Alzheimer's disease diagnosis.
Among the 20 significant species, six were identified as likely risk species and the other 14 potentially protective species for Alzheimer's diagnosis.
Risk genera included Alistipes and Bacteroides from the Bacteroidetes phylum, Lachnospira and Veillonella from the Firmicutes phylum, and Collinsella from the Actinobacteria and Sutterella from the Pseudomonadota phyla. The most significant risk-associated species was Bacteroides.
For protective species, 11 out of 14 were from the Firmicutes phylum, two were from Actinobacteria, and one was from Bacteroidetes (Prevotella 9). The most significant protective genus was Intestinibacter.
These findings alone would make for an interesting paper, but the researchers seemed more interested in doing good science, so they challenged their results with a follow-up analysis.
A second database was used from GenADA, a multi-site Canadian collaboration study of Alzheimer's patients. The same techniques were used to find correlations between the microbiota in 799 cases with 778 controls. The data from this replication study differed from the first in some areas, but where the two experiments overlapped in four significant correlations pointed to the most likely culprit.
APOE4
Apolipoprotein E (APOE) is the central nervous system's major cholesterol and lipid carrier protein. Of the three major human versions of the protein, APOE2, APOE3, and APOE4, the genetic expression of APOE4 is one of the most significant risk factors linked to the development of late-onset Alzheimer's disease.
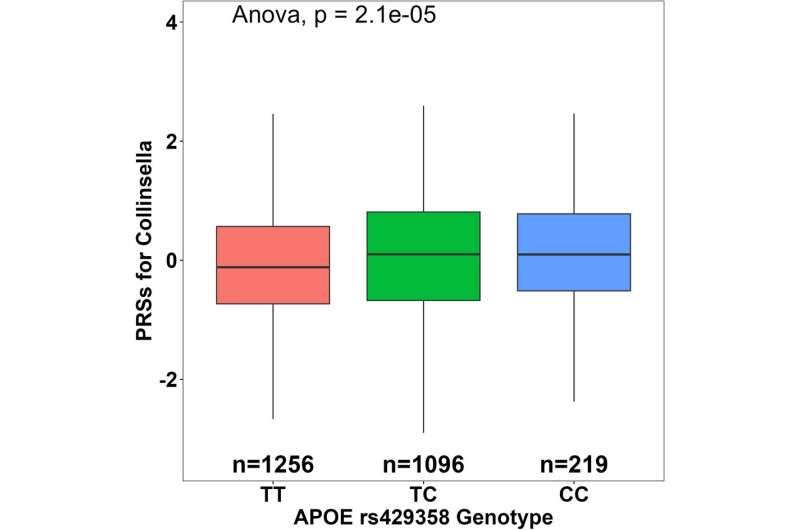
When the researchers looked deeper into the overlapping microbial associations with Alzheimer's, they found that these patients had something else interesting in common. Polygenic risk scores of the four microbiota species had significant associations with a specific version of the APOE genotype rs429358-C.
Collinsella from the phylum Actinobacteria was identified as a risk factor for Alzheimer's in both the discovery and replication samples and had the most significant associations with the APOE genotype at rs429358-C.
The paper points out that previous studies have found that Collinsella correlates with higher serum levels of total cholesterol and low-density lipoprotein (LDL) cholesterol in healthy adults, which the researchers speculate may be connected to interactions between Collinsella and APOE.
The researchers conclude that future research is needed to explore the relationship between Collinsella, lipid metabolism, and inflammatory signals to elucidate how their interaction influences Alzheimer's and other diseases.
More information: Davis Cammann et al, Genetic correlations between Alzheimer's disease and gut microbiome genera, Scientific Reports (2023). DOI: 10.1038/s41598-023-31730-5
© 2023 Science X Network




















