This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
A thick skin: How a very exposed organ fights disease
Humans are just so naked. Where many creatures have scales or spines—or even a shell—humans have a soft, sweaty, stretchy layer of skin standing between the world and our internal organs.
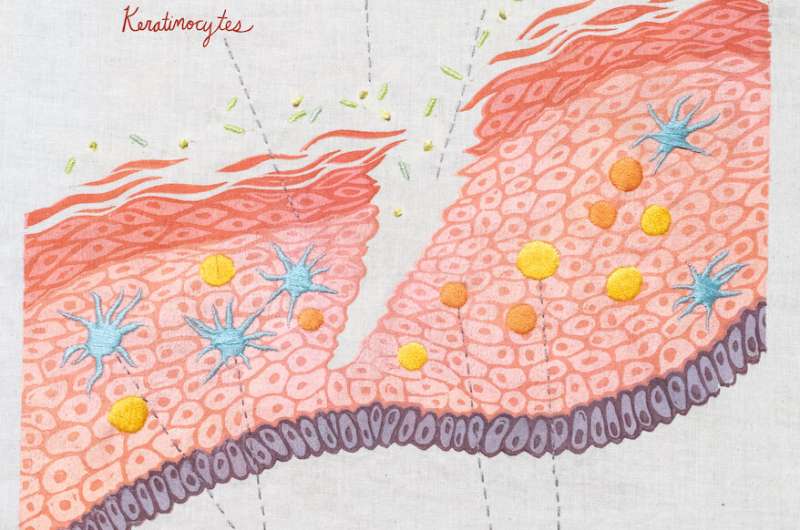
Thank goodness the skin also has an army of immune cells. The main players are keratinocytes, which make up 90 percent of skin cells. These cells produce the proteins (such as keratin) and lipids that make your skin such an effective barrier to the outside world. Keratinocytes make us waterproof. They help us heal from cuts, scrapes, sunburns, and tattoo guns.
Keratinocytes offer immune protection: they can produce antimicrobial peptides, and they can make inflammatory molecules signal other immune cells to defend the skin.
Dotted among the keratinocytes are Langerhans cells. These are really just dendritic cells, a kind of innate immune cell (or first line of defense). Then there are "intradermal" immune cells. These intradermal cells include a large population of T cells, which specialize in detecting foreign molecules, and memory T cells, which remember past infections.
Anyone who's itched a bug bite or touched poison oak has experienced the speed and sensitivity of the skin's immune system. Unfortunately, reactions in the skin also can lead to inflammatory and autoimmune diseases. La Jolla Institute for Immunology (LJI) Professor Michael Croft, Ph.D., studies skin diseases such as atopic dermatitis, the most common type of eczema. His laboratory has discovered important molecules that drive skin inflammation—and helped demystify the immune system of the skin.
"You could argue that some of the immune molecules we study really evolved to help the skin heal itself," says Dr. Croft. "This system activates any time you get a disruption of the skin, like a scratch. Part of the response that may occur in people with skin inflammatory diseases like atopic dermatitis, psoriasis, scleroderma, and similar diseases is really an aberrant or exaggerated wound healing response."
In atopic dermatitis, for example, the immune system of the skin starts to overreact to innocent molecules, such as milk proteins or laundry detergents. Keratinocytes are triggered to react to these inflammatory stimuli and become overactive, just as they would when trying to close a wound. "Keratinocytes divide more than they normally should," says Dr. Croft. "And you start to build up a much thicker epidermis."
This keratinocyte activity is why patches of skin affected by atopic dermatitis, psoriasis, or scleroderma feel thicker or rougher than unaffected areas. A very similar process happens in the airways when an allergen triggers an asthma attack: cells in the airways thicken, worsening breathing issues.
Dr. Croft's laboratory has shown we might bring balance back to the skin by targeting a pair of immune system proinflammatory proteins called TWEAK and LIGHT. These proteins belong to a family of molecules known for causing inflammation throughout the body, and Dr. Croft's research with mouse models of disease as well as human keratinocytes shows they can drive the deregulated keratinocyte activity that is common in most inflammatory and autoimmune diseases of the skin.
Dr. Croft and his colleague, LJI Instructor Rinkesh Gupta, Ph.D., have found that deleting the genes for the receptors of TWEAK or LIGHT found on keratinocytes can protect mice from getting psoriasis and atopic dermatitis. Blocking the activity of TWEAK or LIGHT in mice with neutralizing antibodies also appears to stop psoriasis and atopic dermatitis after the inflammation has started.
"We think both of these molecules are essential to all skin diseases and represent more universal targets for therapeutic treatment in humans," Dr. Croft says.
Dr. Croft points out that keratinocytes aren't very different from the epithelial cells, or barrier cells, that line the airways. "A lot of the barrier surfaces actually have somewhat the same structure and potentially the same mechanisms for healing, as well as producing damage," he says. That means shedding light on inflammation in diseases like asthma may advance skin disease research too—and vice versa. In a recent asthma study, Dr. Croft and his LJI colleagues showed that blocking the activity of LIGHT can stop the kind of tissue thickening seen in the airways of people with severe asthma. So there's good reason to think a similar strategy could lead to healthier skin.
We think of skin as a shield or a barrier, but skin can also be a window into the immune system. Look down at your hands. They've been through cuts and burns, snowball fights and sun damage. Yet keratinocytes close the wounds, immune cells remember past threats, and your skin stands ready for the next challenge.





















