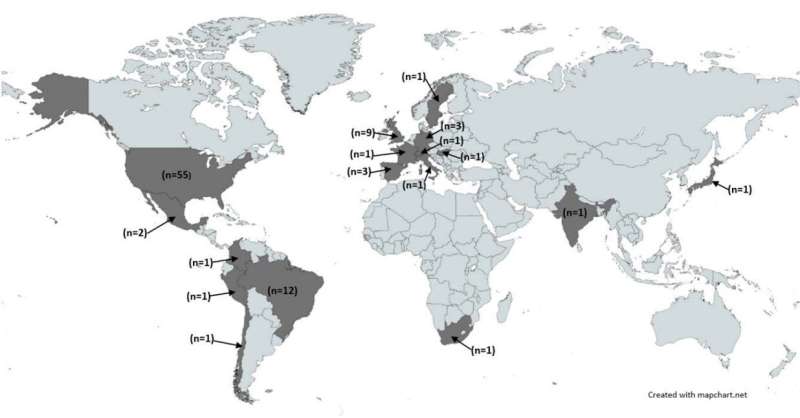
Map of global distribution of included studies. Credit: The Lancet Public Health (2022). DOI: 10.1016/S2468-2667(22)00223-7
Mortality rates of COVID-19 around the globe were higher in areas of socioeconomic disadvantage, new research has revealed.
In a new international review, published in The Lancet Public Health, a study by NIHR School of Public Health researchers at Newcastle University adds evidence to the growing picture of an unequal pandemic, resulting in health inequalities and outcomes.
The experts reviewed 95 studies worldwide and found extensive evidence of more COVID-19 deaths among those living in the most deprived areas.
Importance of leveling-up
A large majority of the studies showed that during the first two years of the pandemic, there were inequalities at every level of geography—neighborhood, town, city, region—where people living in poverty had higher rates of mortality than their more affluent neighbors.
There was evidence of an association between COVID-19 deaths and area-level deprivation in four out of six global regions. Findings are in-line with data on inequalities from other recent pandemics, such as H1N1 influenza, Ebola and Zika.
Lead author on the study, Dr. Vic McGowan, a Research Fellow at Newcastle University, said, "Our review provides clear evidence that those living in the most deprived communities shouldered the greatest burden from COVID-19.
"The leveling-up agenda in the U.K. has the potential to reduce inequalities between areas of high and low deprivation, this would go some way to preventing inequalities arising in future pandemics."
The pandemic took place against a backdrop of social and economic inequalities. Research from England had found large regional inequalities with high rates of COVID-19 deaths in the most deprived northern regions.
However, there has been no assessment of whether there was a similar association in other countries. Therefore, in this new report, researchers sought to explore what is known about geographical inequalities in COVID-19 deaths globally.
Understanding the relationship between COVID-19 mortality rates and deprivation is complex. Deprivation is affected by wider social determinants of health, such as housing, working conditions, unemployment and healthcare access.
These factors can cause higher exposure to the virus, for example, people in low-income jobs are less amenable to remote working so employees were less able to benefit from local lockdown restrictions and working from home. Self-isolation is also harder in overcrowded housing and densely populated areas.
Additional support required
Professor Clare Bambra, co-author of the study, said, "Our research shows that COVID-19 is an unequal pandemic—people in more deprived communities, globally and in the U.K., have been most impacted with higher deaths.
"As we face a possible twindemic of flu and COVID-19 this winter in England, additional support for the NHS in those parts of the country most likely to be adversely impacted should be considered as a matter of urgency.
"Health inequalities between the rich and the poor exist globally. Tackling this requires collaborative cross-government action, for example, working with people who have lived experience of living in deprivation to develop effective solutions."
More information: Victoria J McGowan et al, COVID-19 mortality and deprivation: pandemic, syndemic, and endemic health inequalities, The Lancet Public Health (2022). DOI: 10.1016/S2468-2667(22)00223-7
Journal information: The Lancet Public Health
Provided by Newcastle University