The “Swiss cheese” model of respiratory virus transmission prevention. Credit: Infection Control & Hospital Epidemiology (2022). DOI: 10.1017/ice.2022.295
Health care facilities should no longer routinely screen symptom-free patients for COVID-19 upon admission or before procedures and rely instead on enhanced layers of infection prevention interventions, according to a recommendation from the Society for Healthcare Epidemiology of America (SHEA) published today in Infection Control & Hospital Epidemiology.
"The small benefits that could come from asymptomatic testing at this stage in the pandemic are over ridden by potential harms from delays in procedures, delays in patient transfers, and strains on laboratory capacity and personnel," said Thomas R. Talbot, MD, MPH, the Chief Hospital Epidemiologist at Vanderbilt University Medical Center, and a member of the SHEA Board of Directors. "Since some tests can detect residual virus for a long period, patients who test positive may not be contagious."
The authors, members of the SHEA Board of Directors, noted a lack of evidence that asymptomatic testing reduces health care-associated COVID infections and suggest such testing requirements may disproportionally impact disadvantaged populations who have limited access to care and testing resources.
The authors also cited research that shows asymptomatic COVID testing added 1.89 hours to the length of stay in the emergency department of an academic health system, and another study from a specialty hospital showed it cost more than $12,500 to identify one asymptomatic COVID patient.
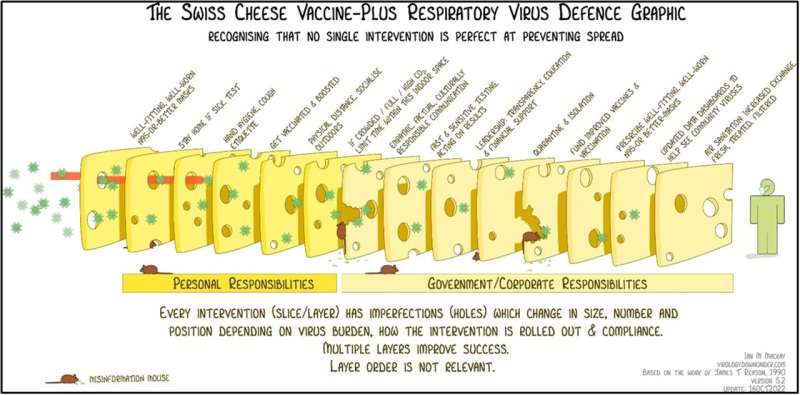
Facility risk assessments that include targeted scenarios, patient populations, or locations that may require added interventions along with community COVID-19 metrics should drive whether asymptomatic screening is part of institutional practices. While it is imperative to prevent health care–associated spread of respiratory pathogens, it is critical to examine which methods, when added upon core layers of infection prevention, work best to protect patients and health care providers.
A hierarchy of controls to prevent infections can include universal use of N95 respirators when performing certain procedures, active screening of health care providers for signs of COVID-19, unit layouts that reduce shared patient spaces, and enhanced cleaning and ventilation.
More information: Thomas R. Talbot et al, Asymptomatic screening for severe acute respiratory coronavirus virus 2 (SARS-CoV-2) as an infection prevention measure in healthcare facilities: Challenges and considerations, Infection Control & Hospital Epidemiology (2022). DOI: 10.1017/ice.2022.295
Provided by Society for Healthcare Epidemiology of America