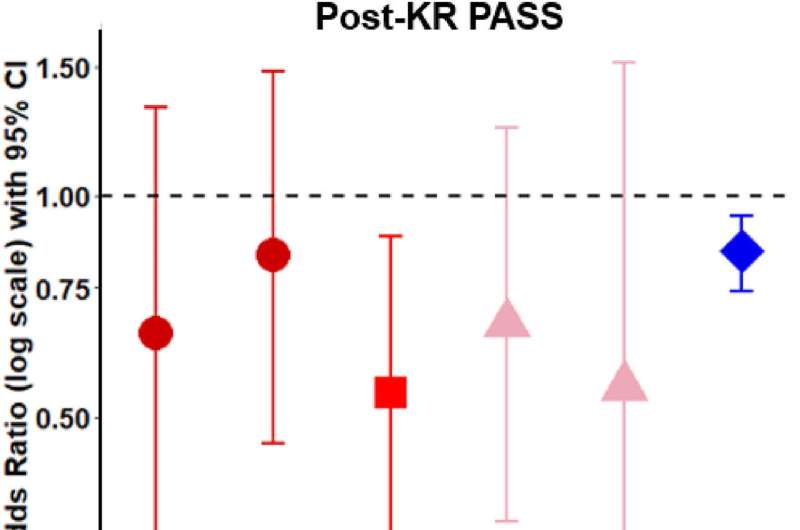
Post-KR relations of altered nociceptive signaling and the number of painful sites to WOMAC pain. Credit: Osteoarthritis and Cartilage Open (2023). DOI: 10.1016/j.ocarto.2023.100335
Knee osteoarthritis (OA) is the most common form of arthritis worldwide, affecting more than 500 million people worldwide and 34 million people in the U.S. There are no treatments available that prevent its progression and recommended pharmacological treatments and other treatments (exercise, weight loss) have either small-to moderate effects or short-term effects. As such, knee replacement (KR) is considered one of few therapies that can considerably improve pain and function in patients with severe, end-stage knee OA.
While a majority of patients experience marked improvement in pain after KR, approximately 20-30 percent of patients continue to experience knee pain post-KR, but why this pain continues to persist is not well-understood.
Now researchers from Boston University Chobanian & Avedisian School of Medicine have determined that altered pain signaling in the nervous system may be persistent even after surgery.
"Because the majority of patients do well when much of the pathologic tissue presumably contributing to symptoms related to OA is removed, pain persistence post-KR suggests that other factors are likely at play," said corresponding author Tuhina Neogi, MD, Ph.D., professor of medicine at the School.
The researchers evaluated 171 participants from the Multicenter Osteoarthritis Study approximately 12 months after KR for measures of pain sensitivity.
They found that presence of certain alterations in nervous system signaling were associated with worse knee pain after KR. They also found that people who had other painful body sites also experienced worse knee pain following KR.
According to the researchers, a clinical implication for these findings is that central pain mechanisms are an important target for pain management and that management of other sites of pain may be important in ameliorating persistent knee pain. Centralized pain mechanisms are associated with changes within the central nervous system that amplify peripheral input and/or contribute to the perception of pain in the absence of a stimulus.
"While we were not able to address this directly, this study raises a question about the timing of knee replacement. It is presently unknown if some of these alterations to central nervous system may become irreversible if present for too long and whether replacing a joint earlier may allow for these signaling changes to normalize," added Neogi, who also is chief of rheumatology at Boston Medical Center.
These findings appear online in the journal Osteoarthritis and Cartilage Open.
More information: Kosaku Aoyagi et al, Post-surgical contributors to persistent knee pain following knee replacement: The Multicenter Osteoarthritis Study (MOST), Osteoarthritis and Cartilage Open (2023). DOI: 10.1016/j.ocarto.2023.100335
Provided by Boston University School of Medicine