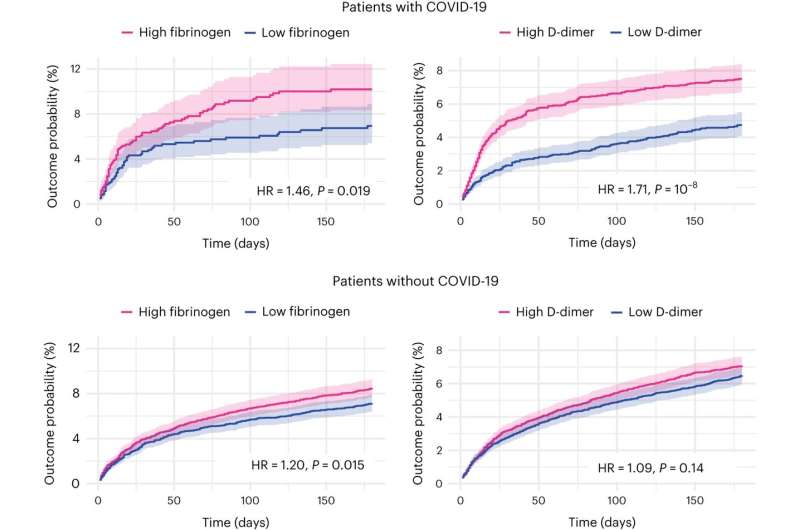
Replication and generalization of the findings using electronic health records data. Kaplan–Meier curves represent the cumulative incidence of cognitive deficits between those with high versus low fibrinogen (or D-dimer) and CRP level ≤10 mg l−1. The same analysis conducted in people without COVID-19 (bottom). Curves represent the Kaplan–Meier estimates and shading around curves represents 95% CI. P values are derived from log-rank tests, are two-sided and not adjusted for multiple comparisons. Credit: Nature Medicine (2023). DOI: 10.1038/s41591-023-02525-y
Two blood biomarkers could be predictive of cognitive deficits six and 12 months after a diagnosis of COVID-19, reports a new study published in Nature Medicine. These findings, based on data from more than 1,800 patients who were admitted to the hospital with COVID-19, were validated in an independent dataset, and provide biological insights into factors that may drive long-term cognitive dysfunction due to COVID-19.
Post-COVID-19 cognitive deficits, including "brain fog," can be debilitating and affect day-to-day life. Their diagnosis includes both objective (clinician-based) components and subjective (patient-reported) components. However, how these post-COVID-19 cognitive deficits develop remains unknown.
Maxime Taquet and colleagues examined data collected from 1,837 patients hospitalized for COVID-19 in the U.K. between 29 January 2020 and 20 November 2021. Blood samples were collected from these patents during admission to the hospital, and both clinician-acquired measurements and patient-reported measurements of cognition were obtained six and 12 months later.
Using a statistical approach, the authors identified two blood biomarker profiles that were highly correlated with post-acute COVID-19 cognitive deficits. The first profile identified high levels of fibrinogen, a protein associated with blood coagulation, that correlated with both objective cognitive deficits and subjective cognitive deficits. The second profile associated elevated levels of another blood-coagulation protein, d-dimer, with subjective cognitive deficits, including "brain fog," but also with fatigue and shortness of breath.
The findings were largely replicated in a separate study of the health records of 17,911 patients in the U.S., including comparison of post-pandemic cohorts versus pre-pandemic cohorts, which the authors suggest demonstrates the specificity of d-dimer for COVID-19.
The authors suggest that their findings may enable the development of models for post-COVID-19 cognitive deficits that could facilitate prognosis and management. However, they note that further research is needed in more cohorts.
More information: Maxime Taquet et al, Acute blood biomarker profiles predict cognitive deficits 6 and 12 months after COVID-19 hospitalization, Nature Medicine (2023). DOI: 10.1038/s41591-023-02525-y
Journal information: Nature Medicine
Provided by Nature Publishing Group