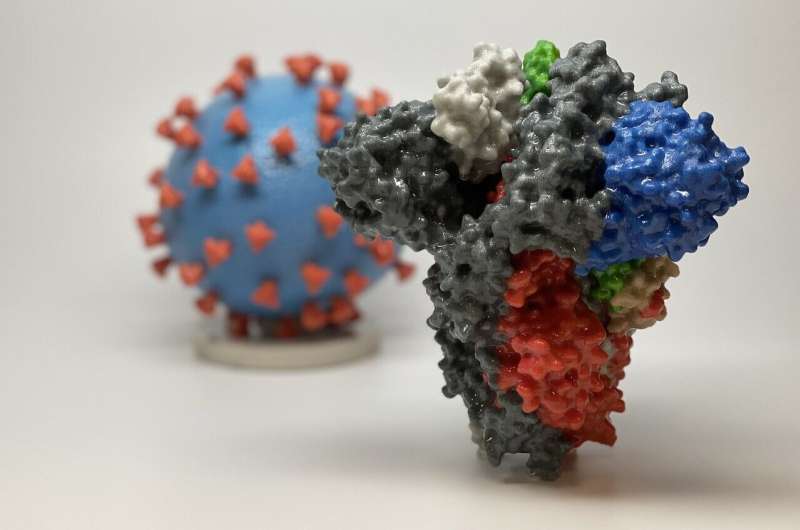
3D print of a spike protein of SARS-CoV-2, the virus that causes COVID-19—in front of a 3D print of a SARS-CoV-2 virus particle. The spike protein (foreground) enables the virus to enter and infect human cells. On the virus model, the virus surface (blue) is covered with spike proteins (red) that enable the virus to enter and infect human cells. Credit: NIH
Researchers at the University of Minnesota and University of Washington found a statistical relationship between the number of hospital beds (ICU and non-ICU) occupied by COVID-19 patients in a state and reported mortality. Published today in the Journal of General Internal Medicine, this research is believed to be the first to use actual, state-level data to examine this association.
"These estimates provide a better understanding of the projections of the COVID-19 pandemic in the U.S. especially when states are monitoring economic activities, and provide important practice insights for hospitals in terms of assessment of hospital bed and ICU bed capacity and preparedness," said study lead Pinar Karaca-Mandic, professor and academic director of the Medical Industry Leadership Institute (MILI) in the U of M's Carlson School of Management.
Utilizing the U of M's COVID-19 Hospitalization Tracking Project, researchers examined data from 23 states that reported daily percentages of ICU and non-ICU-bed use by COVID-19 patients.
The study found:
- COVID-19 patients occupied nearly 20% of all ICU-bed use in all states examined and about a 5% of non-ICU bed capacity;
- a 1% increase in ICU-bed use (17 beds on average) was associated with 2.84 more COVID-19 deaths over the next seven days;
- a 1% increase in non-ICU bed use (130 beds on average) was associated with 17.84 more COVID-19 deaths.
"ICU and non-ICU bed use as a percentage of the bed capacity of a state were significantly associated with an increase of overall COVID-19 deaths over the next seven days," explained Anirban Basu, study co-author and a professor of Health Economics and the director of The CHOICE Institute at the University of Washington. "The intensity of association for ICU-bed use was higher than non-ICU-bed use."
The authors found that the results held true across a variety of alternate specifications.
"Most policy interventions to address the COVID-19 outbreak in the United States have focused on 'flattening the curve' - an approach to spread out hospitalizations over a longer duration to avoid overwhelming the healthcare system," said Soumya Sen, associate professor and academic director of the Management Information Systems Research Center (MISRC) in the Carlson School, who co-authored the study. "The forecasting models informing these policy decisions make assumptions about the relation between the number of COVID-19 cases, hospitalizations, intensive care unit (ICU) demand, and subsequent impact on mortality."
As this study took place during the COVID-19 pandemic, some states may have been able to expand the number of hospital beds. However, the authors note that doing so for ICU beds was likely difficult due to infrastructure constraints.
Other study authors included Dr. Archelle Georgiou, chief health officer of Starkey Hearing Technologies and an executive-in-residence with MILI at the Carlson School, as well as Yi Zhu, a doctoral student at the Information Decision Sciences department in the Carlson School.
More information: Pinar Karaca-Mandic et al, Association of COVID-19-Related Hospital Use and Overall COVID-19 Mortality in the USA, Journal of General Internal Medicine (2020). DOI: 10.1007/s11606-020-06084-7
Journal information: Journal of General Internal Medicine
Provided by University of Minnesota