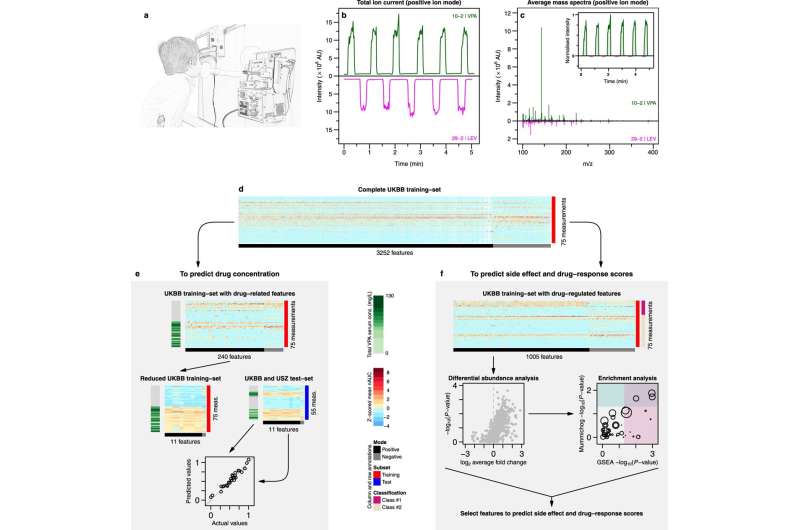
Fig. 1: Overview of the study pipeline. a The procedure begun with a patient performing five-to-six simple exhalations into a SESI–HRMS analytical platform located in the hospital premises. The breath metabolomics fingerprint was acquired in positive and negative-ion mode (5, 6 exhalations per mode). Shortly before the breath test, blood was drawn to evaluate blood/serum concentrations of ASMs. b SESI–HRMS is a real-time, noninvasive, and fast breath-metabolome analysis method. The whole breath test (i.e., positive- and negative-ion mode), lasts typically 10–15 min per patient. Positive-mode TIC from two patients, one receiving VPA and another one receiving LEV, is shown as an example (TIC of patient 29 is inverted to ease visual inspection). c Comparison of the average mass spectra between the two subjects taking VPA and LEV. The inset shows an example of time-trace at m/z 143.1066 (mass spectrum and time-trace of patient 29 inverted to ease visual inspection). For each ion, area under the curve during each exhalation was computed (shaded regions) and normalised by the exhalation time (nAUC). Then, the nAUCs of 5, 6 exhalations were finally averaged to represent mean nAUC of the ion. d This resulted in a 75 × 3252 (measurements × mass spectral features present in at least 10% of total measurements and correlated with exhalations) data matrix (z-score is only used here to ease visual representation; actual downstream analysis was done on raw numbers). e Analysis workflow used to predict VPA serum concentration based on drug-related metabolites. f The workflow used to predict side effects and drug-response scores based on drug-regulated metabolites. See Methods for more detail about panels e and f. Colour key for heatmaps is shown in-between panels e and f. Credit: DOI: 10.1038/s43856-021-00021-3
Epilepsy affects some 50 million people worldwide and pharmaceutical treatment of the disease is a tightrope walk, as the dose must be tailored precisely to the individual patient: "Slightly too little and it isn't effective. Slightly too much and it becomes toxic," explains Professor Pablo Sinues.
Sinues is Botnar Research Professor of Pediatric Environmental Medicine at the University of Basel and University Children's Hospital Basel (UKBB). He is also a member of the Department of Biomedical Engineering at the University of Basel. Together with colleagues from University Hospital Zurich (UHZ), he spent two and a half years looking for a way to tailor the dosage of drugs administered to epilepsy patients as precisely as possible. They ultimately achieved this goal with the help of a breath test. The advantage is that monitoring does not require a blood sample, which can always be a stress factor for children. And as the sample doesn't need to be sent to the laboratory first, the results are available immediately.
Searching for the tiniest concentrations
"You can think of it as being like the alcohol test that police use when they stop drivers," Sinues explains. The difference is that this breath measurement device is actually a big machine. "Because alcohol is present at high concentrations in breath, one only need a small device. But we're searching for a droplet in 20 swimming pools," he says. The researchers want to use the results to determine whether the active substances are present at the right concentrations in the body and whether they have the desired effect on the disease.
Their efforts have not been in vain: both among the young patients at UKBB and the adult reference group at the University Hospital Zurich, the breath tests produced the same results as conventional blood tests, as reported by the research group in their study published in Communications Medicine. This means that in addition to blood tests, there is a second way of monitoring epilepsy treatment—and the method also provides further information on the patient's metabolism that doctors can use in the therapy.
Interdisciplinary collaboration is a recipe for success
The special thing about this research project is the unique dovetailing of science and medical practice at the University of Basel, says Sinues: "Thanks to this favorable initial situation, we are able to build machines that are precisely tailored to the needs of doctors."
At UKBB, the rapid availability of test results is a particular advantage of the new method: young patients require constant adjustments of their medication because their metabolism changes as they grow. The new technology provides doctors with a non-invasive test that gives them immediate clues as to how well the course of therapy is going. This enables them to respond quickly if the dose has to be adjusted.
It took four years to reach this breakthrough and the technique is not yet suitable for widespread use—but that is the goal that Sinues has set himself. Indeed, the start-up Deep Breath Intelligence was founded specifically for that purpose and now aims to obtain a license for the measurement technique.
More information: Kapil Dev Singh et al, Personalised therapeutic management of epileptic patients guided by pathway-driven breath metabolomics, Communications Medicine (2021). DOI: 10.1038/s43856-021-00021-3
Provided by University of Basel