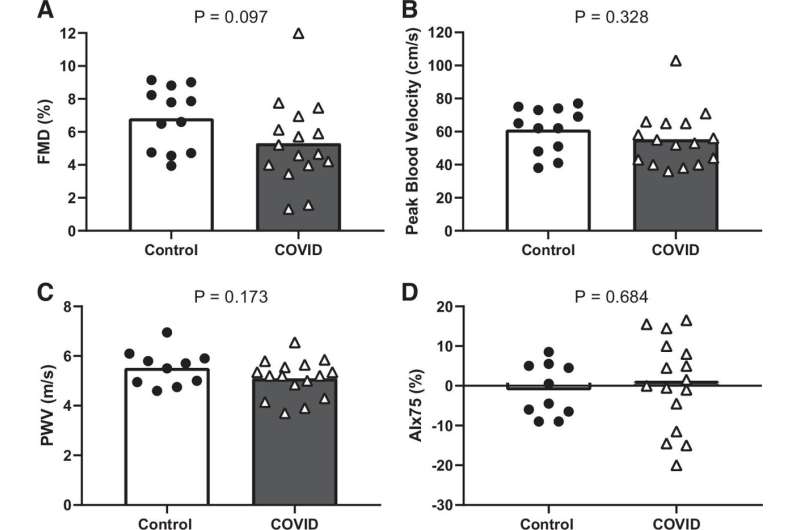
Figure 1. Group means and individual data for flow-mediated dilation (FMD, A), peak blood velocity following cuff release (B) (n = 12 control and n = 16 COVID for both), pulse wave velocity (PWV, C), and augmentation index normalized to heart rate of 75 beats/min (AIx75, D) (n = 10 control and n = 16 COVID for both) between control and COVID groups. Credit: DOI: 10.1152/ajpheart.00368.2021
In a first-of-its-kind study, researchers have examined the persistent effects of SARS-CoV-2 infection on the vascular function of otherwise healthy young adults. The research, published in the American Journal of Physiology-Heart and Circulatory Physiology, was chosen as an APSselect article for September.
Adults 29 and younger make up only 16% of the U.S. population but account for over 7 million, or 22%, of U.S. COVID-19 infections. Though more research is needed to fully understand the extent of the problem, one study found that as many as 1 in 4 adults ages 18 to 39 reported symptoms weeks or months after the initial acute phase of COVID-19 infection.
"Long COVID," also called post-acute sequelae of SARS-COV-2 infection (PASC), is an umbrella term for the condition the U.S. Centers for Disease Control and Prevention refers to as "a lack of return to a usual state of health following acute COVID-19 illness." Individuals with long COVID report a variety of symptoms, including cognitive impairment, headache and lightheadedness, which can be indicative of impairments to blood vessels supporting the brain.
Researchers from University of Texas at Arlington investigated brain and peripheral blood vessel function of 16 young adults who had tested positive for COVID-19 more than four weeks prior. Eight of the study subjects currently had COVID-19 symptoms and eight did not. Researchers then compared them to 12 peers who tested negative.
Credit: American Physiological Society
Symptomatic participants showed "significantly blunted" dilation of both large and small blood vessels in their limbs. However, despite previous studies showing stiffening of central arteries in young adults with acute COVID-19, long COVID participants in this study showed no such stiffening, nor did they show impaired function in the blood vessels that support the brain. Asymptomatic COVID-19–positive participants showed function similar to controls, offering hope that once symptoms resolve so may vascular impairments.
"Blunted peripheral but not cerebral vasodilator function in young otherwise healthy adults with persistent symptoms following COVID-19" is published in the American Journal of Physiology-Heart and Circulatory Physiology.
More information: Damsara Nandadeva et al, Blunted peripheral but not cerebral vasodilator function in young otherwise healthy adults with persistent symptoms following COVID-19, American Journal of Physiology-Heart and Circulatory Physiology (2021). DOI: 10.1152/ajpheart.00368.2021
Provided by American Physiological Society