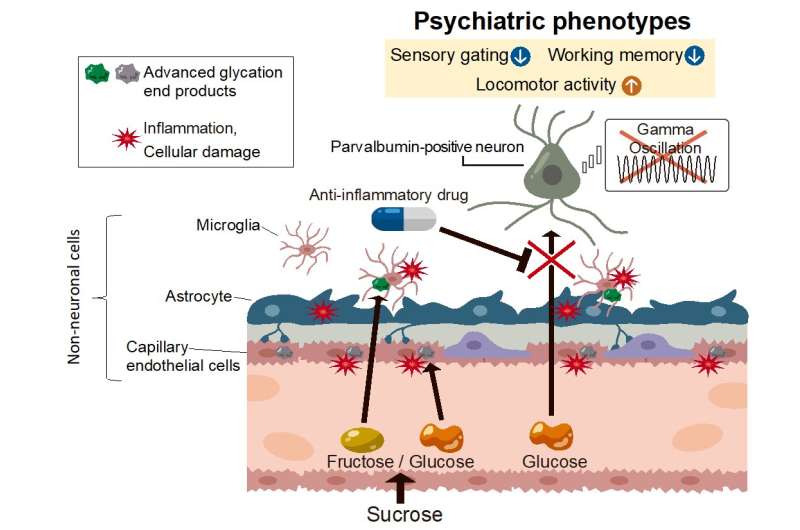
Excessive sucrose intake during adolescence cause cellular damage in non-neuronal cell groups, inhibiting the uptake of glucose from the blood into the brain parenchyma, leading to dysfunctions of certain neurons that cause the major symptoms of psychiatric disorders. Credit: TMIMS
There has been a remarkable increase in intake of simple sugar (sucrose, isomerized sugar (corn syrup) from beverages and diets in modern society. The intake of simple sugars in adolescents, in whom mental disorders frequently occur, is higher than any other generations. Moreover, patients with mental disorders consume approximately 2-fold more sugar than age-matched healthy individuals, and patients with schizophrenia who consume more sucrose exhibit more severe symptoms. Despite accumulating evidence, it is still unproven that excessive sugar intake contributes to the pathogenesis of psychiatric disorders among susceptible individuals. Doesn't an excessive intake of simple sugar affect higher brain function? Researchers have attempted to elucidate this causal relationship.
As a susceptibility gene for psychiatric disorder, the researchers selected Glyoxylase-1 and Disrupted-in-schizophrenia-1. By combining the heterozygous mice with environmental factors of excessive sugar intake at the age of puberty, they successfully created a novel mouse model exhibiting various mental disorder-like symptoms, including decreased sensorimotor gating function, decreased working memory, hyperactivity, abnormal gamma-band component in EEG. In other words, this demonstrates a possibility that the excessive intake of simple sugar at the age of puberty could be an environmental risk factor of psychiatric disorders.
Furthermore, by analyzing this model mouse, the team aimed to identify the new phenotypes and mechanisms of developing mental disorder. They found "cerebral microvascular angiopathy." In order to verify the generality of this finding, they used a post-mortem brain from patients with schizophrenia and bipolar disorder, and identified angiopathy similar to the one seen in the model mice. They also found that the angiopathy was accompanied by an impaired glucose incorporation to brain parenchyma in their mice model. These phenotypes were prevented by continuous administration of non-steroidal anti-inflammatory drugs (NSAIDs) before the onset of the disease, and some psychiatric-like symptoms were also suppressed. Notably, the patients used in this study did not necessarily have a record of excessive sucrose intake. They developed psychiatric disorders under various stress circumstances, suggesting that psychiatric disorders are associated with angiopathy in the brain caused by various environmental stresses, including metabolic stress.
More information: Shinobu Hirai et al, High-sucrose diets contribute to brain angiopathy with impaired glucose uptake and psychosis-related higher brain dysfunctions in mice, Science Advances (2021). DOI: 10.1126/sciadv.abl6077
Journal information: Science Advances
Provided by Tokyo Metropolitan Institute of Medical Science