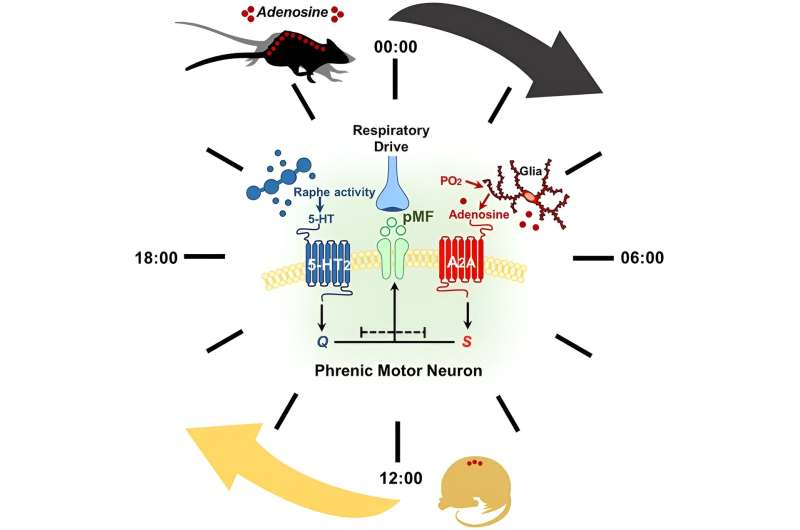
Graphical Abstract The daily rest versus active phase and acute intermittent hypoxia protocol paradigm have profound impact on the magnitude and mechanism of phrenic motor plasticity. Credit: Function (2023). DOI: 10.1093/function/zqad041
Neurochemical mechanisms that enable breathing memory—a form of neuroplasticity (the ability of the nervous system to change its activity in response to injuries) known as phrenic long-term facilitation—are very dependent on the time of day in which acute intermittent hypoxia treatment is delivered, according to researchers from the McKnight Brain Institute at the University of Florida.
Acute intermittent hypoxia is when a person is exposed to alternating periods of normal and low oxygen levels. The "stunning" finding highlights the importance of considering both the method and time of day to administer the therapy. The results are published in a new study in the journal Function.
Researchers believe this study could lead to the improvement of human health in conditions such as spinal cord injuries and ALS, which often result in death from respiratory failure or a lifetime dependence on a ventilator. Both cases result in significant limitations on "quality of life for the patient and their caregivers," Gordon Mitchell, Ph.D., lead author of the study, said.
Researchers have already begun applying the findings of this study to ongoing clinical trials looking at the ability of acute intermittent hypoxia to improve breathing in people with these conditions.
More information: Alexandria B Marciante et al, Magnitude and Mechanism of Phrenic Long-term Facilitation Shift Between Daily Rest Versus Active Phase, Function (2023). DOI: 10.1093/function/zqad041
Provided by American Physiological Society