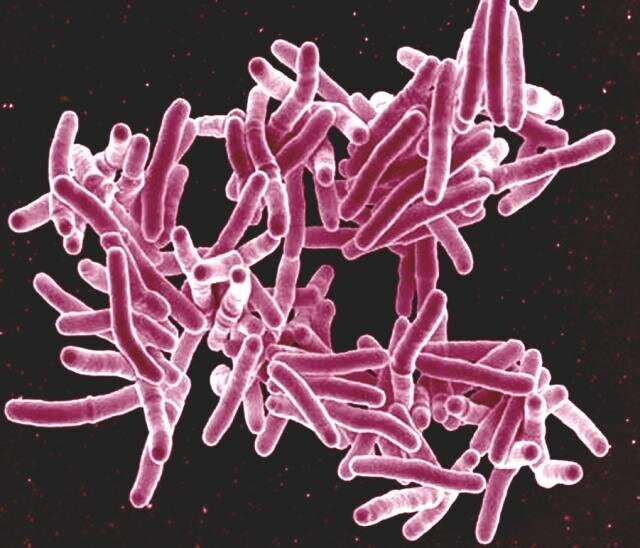
Scanning electron micrograph of Mycobacterium tuberculosis bacteria, which cause TB. Credit: NIAID
Mycobacterium tuberculosis (Mtb), the bacteria that causes a tuberculosis infection, is present in exhaled breath of 90% of those presenting with suspected tuberculosis. This includes those who were negative on conventional sputum testing and not diagnosed with TB. This raises the possibility that those who have tested negative may be unknowingly transmitting the infection.
Researchers from the University of Cape Town and Amsterdam UMC have analyzed results from over 100 patients who presented themselves to clinics in South Africa. These findings are published in PNAS.
"If someone carries Mtb in their respiratory tract, this may also mean they can spread it. Therefore, since these results suggest a much broader range of people transmitting TB than previously recognized, there are significant implications for public health interventions designed to interrupt transmission," says Ben Patterson, external Ph.D. candidate at Amsterdam UMC and the Amsterdam Institute for Global Health and Development.
Participants in the study attended two community clinics in the southwest of Cape Town before being either diagnosed with TB, or not. Subsequently, aerosol samples were collected in a community-based dedicated TB aerobiology lab using a novel method optimized to find low concentrations of Mtb. These samples were then used to detect the presence of Mtb, finding it in the samples given by 90% of patients, including those that had tested negative by sputum for tuberculosis.
"This rather shatters the paradigm on the transmission of tuberculosis. Previously we understood that Mtb was only expelled by those who have the disease, but this study shows that also those with symptoms who test negative do this and probably spread the infection," says Frank Cobelens, professor of Global Health at Amsterdam UMC and senior fellow at the AIGHD.
Aerosol samplings were repeated at three separate timepoints over six months for all participants. The presence of Mtb decreased in those on treatment as well as—surprisingly—those not on treatment over this time period. Nevertheless, 20% of all participants continued to test positively for Mtb in aerosol after six months. This suggests that transmission can continue over a period longer than previously thought. Indeed, a recent study from the University of Cape Town suggests that tuberculosis could be present in the lungs for up to four years prior to the onset of symptoms.
"Together, our results indicate how complex tuberculosis is, and perhaps also why it is so difficult to eliminate tuberculosis in endemic areas. Even when public health agencies work, according to the current guidelines, effectively against symptomatic TB cases. In this sense, a revaluation of our practices is necessary," adds Cobelens.
More information: Aerosolization of viable Mycobacterium tuberculosis bacilli by tuberculosis clinic attendees independent of sputum-Xpert Ultra status, Proceedings of the National Academy of Sciences (2024). On medRxiv: DOI: 10.1101/2022.11.14.22282157
Journal information: Proceedings of the National Academy of Sciences , medRxiv
Provided by Amsterdam University Medical Center