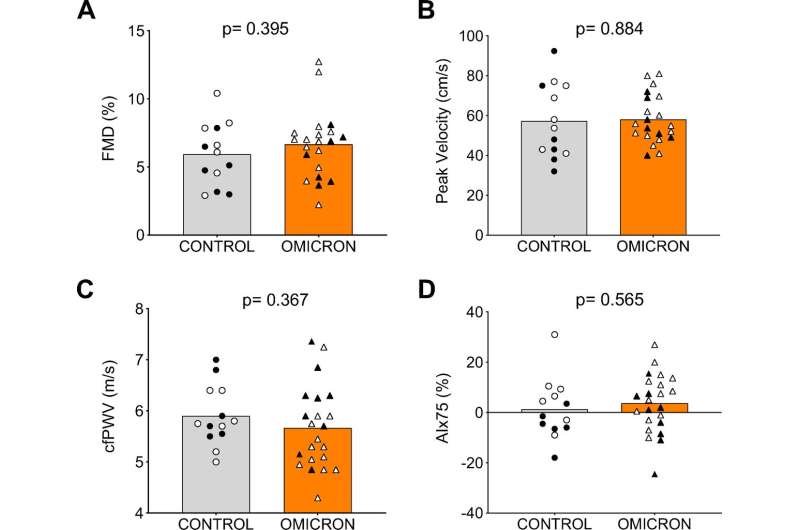
Macro- and microvascular function and arterial stiffness in individuals who never had COVID-19 (control, n = 13; 7 females) and those who had COVID-19 during the Omicron wave (Omicron, n = 23*, 14 females). Males are indicated by black symbols and females by white symbols. A–D: brachial artery flow-mediated dilation (FMD, %; A), reactive hyperemia (peak blood velocity following cuff release, cm/s; B), carotid-femoral pulse wave velocity (cfPWV, m/s; C), and augmentation index (AIx, %; D) corrected for a heart rate of 75 beats/min. Comparisons between groups were made using two-tailed, unpaired t test, and P < 0.05 was used to determine significant differences between groups. *In the Omicron group, n = 21 for FMD and reactive hyperemia and n = 22 for cfPWV. cfPWV, carotid-femoral pulse wave velocity. Credit: American Journal of Physiology-Heart and Circulatory Physiology (2022). DOI: 10.1152/ajpheart.00189.2022
New research finds vaccinated young adults who were diagnosed with COVID-19 during the "omicron wave" of late 2021 and early 2022 did not have lasting vascular impairment after active infection. The first-of-its-kind study is published ahead of print in the American Journal of Physiology-Heart and Circulatory Physiology.
Early COVID-19 research has found that the disease caused by the SARS-CoV-2 virus impairs blood vessel (vascular) health and autonomic function in adults without underlying health conditions even after recovery from active infection. The autonomic nervous system encompasses bodily functions such as digestion and changes in heart rate and respiration rate. The omicron variant of the virus has been shown to cause less severe disease than original strains, particularly in people who have been vaccinated against COVID-19. However, omicron is more transmissible than earlier variants, and many people, although vaccinated, have developed "breakthrough" infections.
Researchers studied a group of young adults in Texas who were diagnosed with COVID-19 between late December 2021 and late January 2022 to determine if the omicron variant causes short-term vascular dysfunction in otherwise healthy, vaccinated adults. All study participants were fully vaccinated at the time of infection, and roughly half of the group had received one booster shot. Although testing did not reveal clearly which variant the volunteers were infected with, research shows that the omicron variant accounted for more than 90% of reported COVID-19 cases in Texas during this time period. None of the volunteers were hospitalized for their illness and all tested positive for COVID-19 an average of 30 days before the study took place.
The research team looked at the participants' blood vessel diameter, blood flow, heart rate and blood pressure to measure vascular and autonomic function. They found no differences in vascular function, arterial stiffness and markers of autonomic function when comparing the COVID-19 group with healthy controls who had not had COVID-19 and were matched for race, age and activity level.
"This finding is likely attributable to the combination of less severity of the omicron variant and vaccination status in these individuals. Considered collectively, these findings are promising given the large numbers of young adults who contracted the omicron variant in late 2021 [or] early 2022," the researchers wrote.
"Impact of breakthrough COVID-19 cases during the Omicron wave on vascular health and cardiac autonomic function in young adults" is published ahead of print in the American Journal of Physiology-Heart and Circulatory Physiology.
More information: Rachel J. Skow et al, Impact of breakthrough COVID-19 cases during the omicron wave on vascular health and cardiac autonomic function in young adults, American Journal of Physiology-Heart and Circulatory Physiology (2022). DOI: 10.1152/ajpheart.00189.2022
Provided by American Physiological Society