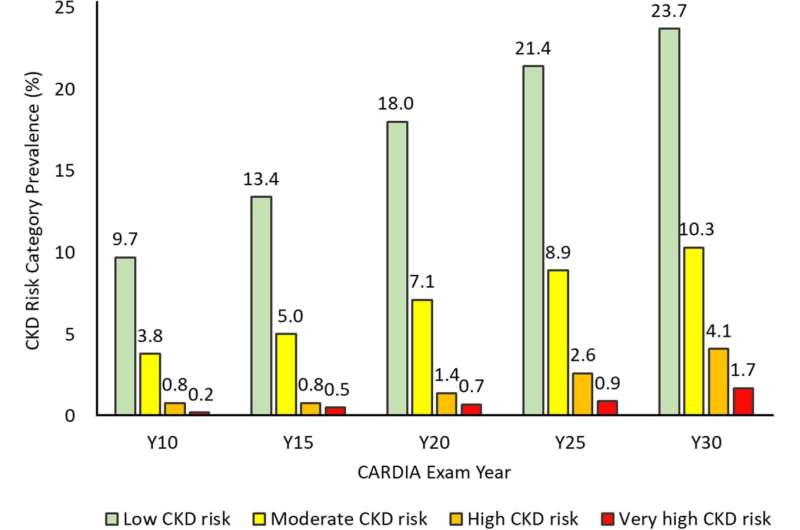
Shift in multinomial CKD risk category prevalence between exam years 10 and 30. Sample size with kidney function markers obtained or found with severe kidney disease on annual followup varied across exams, namely, 3461, 3311, 3369, 3403, and 3010 at exam years 10, 15, 20, 25, and 30, respectively. Cumulative worst CKD risk category for each exam, carrying forward the most recent nonmissing value in the case of missing information, was therefore obtained in 3461, 4032, 4261, 4376, and 4382 participants from exam years 10 to 30 exam. Number of new entries at exam years 15, 20, 25, and 30 were 571, 229, 115, and 6, respectively. Numbers in the very low CKD risk category at exam years 15, 20, 25, and 30 were 2966 (85.7%), 3240 (80.4%), 3113 (73.1%), 2907 (66.4%), and 2651(60.5%), respectively. CKD risk category classification was cumulative over time. Participants were classified in a CKD category at their first attended examination and that classification was updated at the next examination or carried forward if the next examination was missed. CARDIA indicates Coronary Artery Risk Development in Young Adults; and CKD, chronic kidney disease. Credit: Journal of the American Heart Association (2022). DOI: 10.1161/JAHA.122.026685
Researchers from the University of Minnesota School of Public Health (SPH) and Medical School found that 27- to 41-year-olds who experienced kidney function decline tended to have accelerated progression to more severe chronic kidney disease (CKD) and higher risk of cardiovascular disease and death in their middle age, according to a new study, published in the Journal of the American Heart Association.
"These findings add to increasing evidence that maintaining healthy kidney function throughout one's life is important for cardiovascular health and healthy life expectancy," said lead study author Yuni Choi, a postdoctoral researcher at SPH.
The researchers examined data from 4,382 people participating in the Coronary Artery Risk Development in Young Adults (CARDIA) cohort study, tracking test results over a period of 20 years. Study participants ranged in age from 27-41, with an average age of 35 when the study began. Importantly, the researchers tracked the rate at which people in the study progressed through levels of risk for CKD. The key findings of the study are:
- About 28% of people progressed to a higher CKD stage over the course of the two-decade study.
- Higher CKD categories in young adulthood were associated with a greater risk of later experiencing cardiovascular events, including heart attack, stroke, heart failure, or death.
"This study reinforced the fact that young adulthood is a really critical time for clinical attention to the state of the kidneys," said study co-lead author David Jacobs, a professor at SPH. "People who started with a higher CKD stage were more likely to progress to more advanced CKD stages much faster than their peers who started with no CKD or a milder stage of it."
Another interesting finding was the association of CKD stages with cardiovascular disease but not death was explained to some extent by several risk factors, particularly hypertension and diabetes. Whether identified with such other risk factors or in isolation, the findings imply that excess excretion of albumin—a blood plasma protein synthesized in the liver—is an early warning sign for future disease.
"These findings indicate routine monitoring, including of urinary albumin excretion, starting in young adulthood holds promise for initiating and reinforcing prevention of kidney disease, cardiovascular disease, and even death," according to study corresponding author Daniel Duprez, a professor in the U of M Medical School.
The researchers plan to expand on this study to further explore risk factors for CKD progression. They will also conduct a study to analyze racial disparities in CKD disease and surrounding issues.
More information: Yuni Choi et al, Progression of Chronic Kidney Disease Risk Categories and Risk of Cardiovascular Disease and Total Mortality: Coronary Artery Risk Development in Young Adults Cohort, Journal of the American Heart Association (2022). DOI: 10.1161/JAHA.122.026685
Journal information: Journal of the American Heart Association
Provided by University of Minnesota